WellSense Health Plan – New Hampshire wellsense.org
Network Notifications
New Hampshire
Date:
September 30, 2022
Number: 75
To:
All WellSense Providers
From:
WellSense Health Plan
Subject:
September Medical Policy Network Notifications
Product:
☒ NH Medicaid ☒ NH Medicare Advantage
September Network Notifications
The following Well Sense Health Plan medical policies will be updated with revisions to clinical review
criteria and/or applicable coding included in the medical policies (excluding industry-wide code
updates and/or codes that do not require prior authorization). The revised medical policies will be
effective on December 1, 2022:
1. Clinical Review Criteria, OCA 3.201
2. Complementary and Alternative Medicine, OCA 3.194
3. Gender Affirmation Services, OCA 3.11
4. Occupational Therapy in the Outpatient Setting, OCA 3.543
5. Pelvic Floor Stimulation for the Treatment of Incontinence and/or Overactive
Bladder, OCA 3.561
6. Physical Therapy in the Outpatient Setting, OCA 3.544
7. Sacral Nerve Stimulation, OCA 3.563
8. Speech Therapy, OCA 3.542
9. Temporomandibular Joint Disorders, OCA 3.968
General Information
All Well Sense Health Plan medical policies are located on the Provider’s page at
https://www.wellsense.org/providers/nh/policies under the Policies link. If you do not have Web
WellSense Health Plan – New Hampshire wellsense.org
Network Notifications
New Hampshire
access, you may contact your provider relations representative for a copy of the policies. The
updated policies listed above will be posted on the website and available from your provider relations
representative on October 1, 2022.
Questions?
If you have any questions about this Network Notification, please contact your dedicated provider
relations consultant or call the Provider Line at 877-957-1300, option 3 (for NH Medicaid) or 866-
808-3833 (for Medicare Advantage). Well Sense Health Plan Network Notifications and
Reimbursement Policies are available online at wellsense.org.
Clinical Review Criteria
1 of 33
Administrative Policy
Clinical Review Criteria
Policy Number: OCA 3.201
Version Number: 30
Version Effective Date: 11/01/22
Impacted Products
☒ All Products
☒ NH Medicaid
☒ NH Medicare Advantage
☒ MA MassHealth ACO
☒ MA MassHealth MCO
☒ MA Qualified Health Plans/Employer Choice Direct
☒ MA Senior Care Options
Note: Disclaimer and audit information is located at the end of this document.
Policy Summary
This policy defines the Plan’s process for making utilization review decisions using written clinical
review criteria based on sound and current clinical evidence. The Plan conducts all utilization review
activities in accordance with applicable policies and procedures and the Plan’s Utilization Management
(UM) Program. Plan-adopted written clinical review criteria are used to determine the medical
necessity of services that require utilization review, including medical services, surgical treatment,
pharmacotherapy and pharmacy services, behavioral health services, radiological services, dental
services, and durable medical equipment, prosthetics, orthotics and supplies (DMEPOS). In addition,
clinical review criteria are used to determine the most clinically appropriate level of care and intensity
of services to ensure the provision of medically necessary services. Plan-adopted written clinical
review criteria include the Plan’s internally developed medical and pharmacy policies, InterQual®
criteria, and clinical guidelines established by delegated management partners (for related services
provided to Plan members for applicable Plan products). All Plan-adopted written clinical review
criteria are reviewed at least annually and are developed in accordance with contractual requirements,
state and federal regulations, and guidelines from accrediting organizations, including National
Committee for Quality Assurance (NCQA). Review the Plan’s Prior Authorization/Notification
Requirements Matrix, Code Look-up Tools, medical and pharmacy policies, and the Plan’s pharmacy
formulary (available via the drug search tool or the formulary guidebook) to determine if prior
authorization is required.

Clinical Review Criteria
2 of 33
The Plan’s clinical coverage criteria and UM decision tools are applied equitably across the Plan’s
membership. However, the Plan’s Office of Clinical Affairs (OCA) UM staff (or the delegated clinical
vendor’s professional staff when the management of services is delegated to the vendor) will take into
account the member’s individual needs, circumstances, and healthcare services requested and/or
currently provided to the member to integrate healthcare for continuity, coordination, and
collaboration of services, as well as assessing the local healthcare delivery system’s ability to meet the
member’s healthcare needs, when determining the medical necessity of services. Plan guidelines
(including but not limited to appeals and/or clinical reconsiderations) comply with all applicable Plan
contract terms with providers, employers, governmental agencies, and other contracting entities.
The Plan complies with coverage guidelines for all applicable state and federally-mandated benefits.
Plan authorizations, as well as authorizations by each of the Plan’s delegated clinical vendors
conducting utilization management, are based on a comprehensive and individualized needs
assessment that addresses all member needs, including but not limited to social determinants of health
and a subsequent person-centered planning process. Plan prior authorization requirements (and those
of each of the Plan’s delegated clinical vendors) comply with parity in mental health and substance use
disorders. The Plan and the Plan’s delegated clinical vendors conducting utilization management do
NOT discriminate, arbitrarily deny, or impose stricter requirements by reducing the amount, duration,
or scope of required and medically necessary services for ANY Plan member based on the member’s
diagnosis, type of illness, health status or condition, sex, gender identity or dysphoria, or sexual
orientation.
See the member’s product-specific handbook on the Plan’s website for benefit coverage guidelines
and a summary of member rights and responsibilities, as well as the Plan’s process for receiving and
promptly resolving inquires, grievances, or appeals from a member (or an authorized representative
acting on behalf of the member). Member appeals may be related to issues that include but are not
limited to benefit coverage, the evaluation of clinical technology (including new technology and a new
indication for an established technology), and/or the application of the Plan’s clinical review criteria for
the member’s requested indication for treatment.
The Plan’s Cosmetic, Reconstructive, and Restorative Services medical policy, policy number OCA 3.69,
includes the product-specific definitions of cosmetic services and reconstructive surgery and
procedures. The product-specific definitions of experimental or investigational treatment are listed in
the Plan’s Experimental and Investigational Treatment medical policy, policy number OCA 3.12.
Product-specific definitions for medically necessary services (i.e., medical necessity) are listed in the
Plan’s Medically Necessary medical policy, policy number OCA 3.14. The Clinical Technology Evaluation
administrative policy, policy number OCA 3.13, outlines the Plan’s process for evaluating new
technology and new clinical application(s) of existing technology. Review the Plan’s applicable
reimbursement policy for payment guidelines related to clinical trials.
Policy Statement
When the Plan conducts utilization review (UR), appropriate professional utilization management (UM)
Plan staff consistently apply current, Plan-adopted written clinical review criteria, including the Plan’s
Clinical Review Criteria
3 of 33
internally developed criteria specified in internal medical policies and Plan pharmacy policies,
InterQual® criteria, and clinical guidelines established by delegated management partners (for related
services provided Plan members for applicable Plan products). Plan staff (including but not limited to
representatives from the Plan’s Accreditation, Utilization Management, Pharmacy, and Vendor
Management Departments) routinely collects and reviews documentation to verify that quality
standards are met by clinical vendors who are delegated to conduct utilization management on behalf
of Plan members, including but not limited to contractual obligations and the guidelines specified in the
Delegated Management section of this policy. When national clinical guidelines (e.g., InterQual®
criteria) are not available or not adopted by the Plan, Plan-specific criteria may be established and
documented in internally developed medical and pharmacy policies.
The development and review of the Plan’s internal clinical criteria include input from participating
practitioners and consultant specialists in the related specialties that may include but are not limited to
licensed pharmacists, community-based providers, behavioral health clinicians, and physician
specialists in neonatology, pediatrics, family medicine, internal medicine, medical/pediatric/surgical
subspecialties, and geriatrics. Practitioners with professional expertise and relevant credentials in the
clinical area being reviewed have the opportunity to advise or comment on the development, adoption,
and implementation of all UM criteria utilized by the Plan; this includes feedback from qualified
practitioners on staff at the Plan or delegated clinical vendors, outside physician consultants, provider
reviewers, participating providers in the Plan’s network, and practitioners treating Plan members. The
Plan-adopted written clinical review criteria (i.e., the Plan’s internal medical policies and pharmacy
policies, InterQual® criteria, and clinical guidelines implemented by the Plan’s delegated management
partners for related services provided Plan members by Plan product type) are objective, scientifically
derived, and evidence-based for the requested service(s) and indication(s) for treatment and are
compliant with applicable legal obligations , regulatory requirements, and national accreditation
organization standards.
The Plan’s clinical coverage criteria and UM decision tools are applied equitably across the Plan’s
membership. All Plan-adopted written clinical review criteria (including criteria specified in the Plan’s
internal medical policies and pharmacy policies, InterQual® criteria, and clinical guidelines developed
and implemented by the Plan’s delegated management partners for related services provided Plan
members by Plan product type) are clinically reviewed at least annually to verify that these clinical
guidelines are developed and implemented in accordance with generally accepted standards of
medical/clinical practice which are based on objective and credible scientific evidence published in
peer-reviewed medical literature generally recognized by the relevant medical community, relying on
controlled clinical trials. On at least an annual basis, Plan staff confirm that all clinical review criteria
utilized by the Plan (including all of the Plan’s internal medical and pharmacy policies, InterQual®
criteria, and clinical guidelines implemented by the Plan’s delegated management partners for related
services provided Plan members by Plan product type) have had an annual clinical review and the
procedures for applying those clinical review criteria are documented.
Updates to clinical review criteria are implemented as new treatments, applications, and technologies
are adopted and become components of generally accepted professional practice for behavioral
health, medical/surgical services, dental services, and/or pharmacotherapy. The Plan’s Office of

Clinical Review Criteria
4 of 33
Clinical Affairs (OCA) UM staff applies the clinical review criteria consistently; however, OCA UM staff
also takes into account the member’s individual needs and circumstances. The Plan’s Medical
Directors and/or licensed Plan pharmacists consider member-specific factors when applying clinical
criteria to a request for services. When clinical review criteria are not met for a requested treatment
such that medical necessity cannot be established for the member’s condition or indication for
treatment, OCA UM staff engages in discussions with licensed Plan pharmacists, OCA UM clinicians,
and/or Plan Medical Directors to determine if the clinical review criteria are appropriate for the
member’s circumstances or local delivery system (utilizing qualified Plan clinicians applicable for the
member’s condition and requested treatment). If the clinical review criteria are not appropriate, OCA
UM staff may make the utilization determination based on the member’s condition and other unique
circumstances. The Delegated Management section of this policy includes delegated management
guidelines applicable for the Plan’s partner clinical vendors, including Plan oversight and the
development, review, and application of the clinical vendors’ clinical review criteria.
Change Health staff analyze over 3,000 medical literature sources daily to review and update current
InterQual® clinical review criteria and to develop criteria for new technologies and new application(s) of
existing technologies. InterQual® criteria are developed and implemented in accordance with generally
accepted standards of medical/clinical practice which are based on objective and credible scientific
evidence published in peer-reviewed medical literature generally recognized by the relevant medical
community, relying on controlled clinical trials. In addition, InterQual® criteria are evaluated by an
independent clinical review panel drawn from more than 900 experts for authoritative peer review,
utilizing providers with expertise and appropriate credentials in the applicable clinical area under
consideration. Inter-rater reliability testing is conducted annually by the Plan using the Plan-adopted
InterQual® criteria sets. InterQual® criteria are revised, as necessary, throughout the year (at least
annually but may occur quarterly).
Delegated Management
The Plan’s delegated clinical vendors conduct utilization management for behavioral health services,
radiology services, pharmacy services, dental services, and durable medical equipment, prosthetics,
orthotics and supplies on behalf of Plan members (when applicable for the Plan product). Practitioners
with clinical expertise in the area being reviewed have the opportunity to advise or comment on the
development, adoption, and implementation of utilization management criteria established by the
Plan’s delegated management partners; this includes feedback from qualified practitioners on staff at
the Plan or delegated clinical vendors, outside physician consultants, provider reviewers, participating
providers in the Plan’s network, and practitioners treating Plan members.
All Plan-adopted written clinical review criteria, including clinical guidelines established by delegated
management partners, are reviewed at least annually (or more frequently when policy revisions require
more immediate implementation). Clinical review criteria utilized by the Plan’s delegated clinical
vendors are develop with oversight by the clinical vendor’s Medical Director who is an actively
practicing physician and who is responsible for the oversight of the clinical vendor’s utilization
management program. Proposed new and revised clinical guidelines are evaluated by the clinical
vendor’s expert panel, all of whom are practicing clinicians and acknowledged experts in the relevant
Clinical Review Criteria
5 of 33
fields and pertinent specialties. All clinical review criteria are developed in accordance with applicable
state and federal requirements and guidelines from applicable national accreditation organizations.
The clinical review criteria and UM decision tools from each of the Plan’s delegated clinical vendors are
applied equitably across the Plan’s membership. However, the delegated clinical vendor’s professional
staff (when the management of services is delegated to the clinical vendor) will take into account the
member’s individual needs, circumstances, and healthcare services requested and/or currently
provided to the member to integrate healthcare for continuity, coordination, and collaboration of
services, as well as assessing the local healthcare delivery system’s ability to meet the member’s
healthcare needs, when determining the medical necessity of services. Inter-rater reliability testing is
utilized by the Plan’s delegated clinical vendors to assess the consistency and adherence to clinical
review criteria. At least quarterly, the consistency with which the healthcare professionals involved in
prior authorization apply criteria in decision making is evaluated by the delegated clinical vendors using
a variety of mechanisms. The application of medical necessity criteria by Medical Directors and non-
physician reviewers are assessed to ensure consistency and accuracy in the application of the clinical
review criteria. Results are reported to the Plan.
Below are delegated management guidelines applicable for the Plan’s partner clinical vendors,
including Plan oversight and the development, review, and application of the clinical vendors’ clinical
review criteria, as specified below in items 1 through 3:
1. Plan’s Delegated Services and Partner Clinical Vendors:
When applicable for the Plan product, the following services are managed by a delegated
clinical vendor for a Plan member, as stated in items a through f:
a. Behavioral Health Services (Beacon Health Strategies, LLC):
Effective March 1, 2010, the Plan delegated management of behavioral health services to an
NCQA-accredited managed behavioral health organization (MBHO), Beacon Health
Strategies, LLC. The MBHO has its own clinical criteria policy which has been approved as
part of delegation oversight.
b. Dental Services (DentaQuest for Senior Care Options Members):
Effective June 18, 2015, the Plan delegated dental services to Dental Service of
Massachusetts, Inc. (DSM) for DentaQuest to administer the Senior Care Options (SCO)
dental benefit. This clinical vendor establishes policies for communicating criteria to
providers and the vendor has its own clinical criteria policy and procedure which has been
approved as part of delegation oversight.
c. Dental Services (Delta Dental for Qualified Health Plan Pediatric Members):
Clinical Review Criteria
6 of 33
Effective November 23, 2016, the Plan delegated dental services to Dental Service of
Massachusetts, Inc. (DSM) for Delta Dental to administer the Qualified Health Plans (QHP)
pediatric dental benefit. This clinical vendor establishes policies for communicating criteria
to providers and DSM has its own clinical criteria policy and procedures which have been
approved as part of delegation oversight.
d. Durable Medical Equipment, Prosthetics, Orthotics and Supplies (Northwood, Inc.):
Effective April 1, 2011, the Plan delegated management of durable medical equipment,
prosthetics, orthotics and supplies (DMEPOS) to a URAC-accredited DMEPOS clinical
vendor, Northwood, Inc. The Plan has retained the management of medical necessity denial
decisions and notifications. This clinical vendor has its own clinical criteria policy and
procedure which has been approved as part of delegation oversight.
e. Pharmacy Benefits Manager (Express Scripts):
Effective January 1, 2021, Express Scripts is the Plan’s pharmacy benefits manager for the
Plan’s products. Express Scripts adopts the guidelines included in this Plan’s Clinical Review
Criteria administrative policy and adheres to the Plan’s administrative UM policies and
clinical policy criteria, unless specifically delegated such as the Plan’s Medicare product
lines. Policies delegated to Express Scripts have been approved as part of delegation
oversight. Effective December 1, 2019, the Plan’s pharmacy mail order company for all of
the Plan’s Massachusetts and New Hampshire products is Cornerstone Health Solutions.
f. Radiology Services, Musculoskeletal Services, Genetic Testing, and Outpatient
Rehabilitation Services (AIM Specialty Health):
For dates of service on or after November 1, 2022, the Plan has delegated the management
of radiology services, musculoskeletal services (i.e., spine surgeries, joint surgeries, and
interventional pain management treatments), and genetic testing to an NCQA-accredited
managed care clinical vendor, AIM Specialty Health. AIM manages outpatient rehabilitation
services (i.e., physical therapy, occupational therapy, and speech therapy after the initial
evaluation) provided to Plan members for dates of services on or after December 1, 2022.
AIM develops and utilizes criteria to make utilization management decisions for requested
services, establishes policies for communicating those criteria to providers and members,
and evaluates consistency in the application of those criteria through inter-rater reliability
testing when determining medical necessity for these delegated services.
2. Clinical Vendor Clinical Review:
a. Review and Application of Clinical Vendor’s Established Clinical Review Criteria:
The Plan’s Clinical Vendor Oversight Committee conducts an annual review of each clinical
vendor that conducts delegated management for Plan members to ensure that all of the
Clinical Review Criteria
7 of 33
following guidelines are met: each clinical vendor conducts an annual review of its clinical
criteria, approving and implementing criteria that are objective, scientifically-derived, and
evidence-based for the requested service(s) and indication(s) for treatment and compliant
with applicable legal obligations; each clinical vendor completes an annual review and
approval of policies and procedures developed to ensure that the clinical vendor’s clinical
criteria are consistently applied to Plan members for a requested service. The service may
include a treatment, procedure, supply, device, biologic, or drug that will be used to prevent,
diagnose, stabilize, or treat a disease, condition, or disorder that results in health impairment
or disability, or the service allows the member to attain, maintain, or regain functional
capacity. The clinical vendor will also consider member-specific factors impacting the
member’s individual healthcare needs when applying clinical review criteria to determine if
the service is medically necessary for the requested indication. Individual consideration
includes an assessment of any member-specific factor impacting care, including one or
more of the following:
(1) Member’s condition;
(2) Member’s comorbidities;
(3) Member’s age, including the assessment of the member’s age-appropriate growth,
development, and competencies, as well as evaluation of age-related and condition-
specific healthcare needs and associated issues;
(4) Relevant past medical/surgical/behavioral health/dental/pharmacotherapy history;
(5) Complications;
(6) Progression of the member’s condition, illness, or injury;
(7) Diagnostic test results;
(8) Treatment outcomes;
(9) Treatment options;
(10) Psychosocial circumstances;
(11) Home and environmental factors impacting member’s clinical condition (e.g.,
homelessness, employment status, poverty, neighborhood);
(12) Other healthcare services requested and/or provided to the member to integrate
healthcare for continuity, coordination, and collaboration of services;
Clinical Review Criteria
8 of 33
(13) Local healthcare delivery system’s ability to meet the healthcare needs of the
member’s specific condition;
(14) Member’s reasonable accessibility to a qualified provider with appropriate credentials,
licensure, clinical expertise and/or resources in the applicable clinical area necessary
to adequately manage the member’s condition (including but not limited to
pharmacotherapy, behavioral health services, dental services, radiology services,
and/or durable medical equipment, prosthetics, orthotics and supplies);
(15) Other factors related to the member’s plan of care or health outcomes; AND/OR
(16) If applicable, verification that the requested device, therapeutic, biologic, or drug is
being prescribed/requested and will be utilized according to its FDA-approved or
compendia indication and guideline information, including intended use for the
member’s age and medical condition.
b. Clinical Vendor Review of Requested Service Without Written Clinical Review Criteria:
If written clinical review criteria have not been established for the requested service (for the
specified indication) by the Plan’s delegated management clinical vendors, these clinical
vendors will use published and applicable generally accepted, scientifically-based standards
of care and objective and credible scientific evidence published in peer-reviewed
medical/clinical literature, and/or reviewing observational studies for a request for services
for a Plan member to make medical necessity determination. If scientifically-based
standards of care are not available, observational studies from more than one (1) institution
that suggest a causal relationship between the service or treatment and health outcomes
may be used by the delegated utilization management clinical vendor to make medical
necessity determinations if these observational studies are clinically appropriate with
respect to the member’s clinical presentation. The Plan’s delegated management clinical
vendors will also consider member-specific factors impacting the member’s individual
healthcare needs to determine if the service is medically necessary for the requested
indication. The service may include a treatment, procedure, supply, device, biologic, or drug
and will be used to prevent, diagnose, stabilize, and/or treat a disease, condition, and/or
disorder that results in health impairment and/or disability, and/or the service allows the
member to attain, maintain, or regain functional capacity. Individual consideration includes
an assessment of any member-specific factors impacting care, including one or more of the
following:
(1) Member’s condition;
(2) Member’s comorbidities;
Clinical Review Criteria
9 of 33
(3) Member’s age, including the assessment of the member’s age-appropriate growth,
development, and competencies, as well as evaluation of age-related and condition-
specific healthcare needs and associated issues;
(4) Relevant past medical/surgical/behavioral health/dental/pharmacotherapy history;
(5) Complications;
(6) Progression of the member’s condition, illness, or injury;
(7) Diagnostic test results;
(8) Treatment outcomes;
(9) Treatment options;
(10) Psychosocial circumstances;
(11) Home and environmental factors impacting member’s clinical condition (e.g.,
homelessness, employment status, poverty, neighborhood);
(12) Other healthcare services requested and/or provided to the member to integrate
healthcare for continuity, coordination, and collaboration of services;
(13) Local healthcare delivery system’s ability to meet the healthcare needs of the
member’s specific condition;
(14) Member’s reasonable accessibility to a qualified provider with appropriate credentials,
licensure, clinical expertise or resources in the applicable clinical area necessary to
adequately manage the member’s condition, including but not limited to
pharmacotherapy, behavioral health services, dental services, radiology services, or
durable medical equipment (prosthetics, orthotics and supplies);
(15) Other factors related to the member’s plan of care or health outcomes; AND/OR
(16) If applicable, verification that the requested device, system, biologic, or drug is being
prescribed/requested and will be utilized according to its FDA-approved or
compendia indication and guideline information, including intended use for the
member’s age and medical condition.
c. Clinical Vendor Evaluation of New Technology:
The Plan’s partner clinical vendors evaluate new technology and new application(s) of an
established technology to develop new clinical review criteria or revise established clinical

Clinical Review Criteria
10 of 33
review criteria when clinically appropriate. The Plan’s partner clinical vendor will use
published and applicable generally accepted, scientifically-based standards of care and
objective and credible scientific evidence published in peer-reviewed medical/clinical
literature, and/or reviewing observational studies for the new technology or new
application(s) of an existing technology to establish written clinical review criteria that will
be used to make medical necessity determinations (in addition to individual consideration of
the member’s status and healthcare needs). When a requested service that does not have
established, applicable clinical review criteria, the medical necessity of the service is
determined on a case-by-case basis for individual consideration, as specified above in the
Clinical Vendor Review of Requested Service Without Written Clinical Review Criteria
section.
d. Out-of-Network Providers:
The clinical vendor will authorize a member’s care from an out-of-network provider when, as
determined by the clinical vendor, the care and necessary resources are needed by the
member are not available or are not reasonably accessible to the member.
e. Input from Practicing Practitioners:
Actively practicing practitioners with appropriate credentials and clinical expertise in the
applicable clinical area have the opportunity to submit comments on clinical review criteria
utilized by clinical vendors who are delegated to conduct utilization management on behalf
of Plan members (with feedback related to the development, ongoing management, and/or
application of those criteria). Practitioners may submit feedback through the Plan’s
Provider Information Mailbox available at Provider.Info@BMCHP-wellsense.org.
If the practitioner would like to provide input on a clinical vendor’s clinical review criteria and
have those comments considered during the criteria’s next annual review, supporting
documentation must be provided that includes position statements developed or endorsed
by nationally recognized professional associations, consensus reports or guidelines from
specialty societies, and/or standards adopted by governmental agencies (e.g., National
Institutes of Health, Agency for HealthCare Research and Quality, Center for Medicare &
Medicaid Services, Massachusetts Executive Office of Health and Human Services, or New
Hampshire Department of Health and Human Services). Published scientific evidence from
additional reputable sources may also be submitted for consideration.
Issues related to clinical review criteria that must be addressed before each clinical vendor’s
annual review will be evaluated immediately during a prior authorization request for services;
clinical vendors conducting delegated utilization will engage in individual case discussions
with qualified clinicians applicable for the member’s condition and requested treatment to
determine if the clinical review criteria are appropriate for the member’s circumstances or
care provided by a local delivery system according to the guidelines specified below in the
Application of the Plan’s Clinical Review Criteria section of this policy.

Clinical Review Criteria
11 of 33
f. Access to Clinical Review Criteria:
The Plan makes all of its clinical review criteria available to practitioners and members upon
oral or written request. Providers and member may call or fax the Plan with a request for a
copy of the specific criteria, as stated in writing in the provider manual on the Plan’s website.
This access to clinical review criteria includes applicable copyrighted commercial criteria
used by the Plan’s partner delegated clinical vendors. Participating providers are notified at
least 60 calendar days before the implement of substantive revisions to applicable coding
(excluding industry-wide code updates) and/or clinical review criteria (i.e., implementation
of new medical necessity guidelines and/or revised clinical review criteria) used by the
Plan’s partner delegated clinical vendors. The current version of clinical review criteria is
available to all providers, members, and the general public on the Plan’s extranet site.
3. Plan Oversight:
Plan staff (including but not limited to representatives from the Plan’s Accreditation, Utilization
Management, Pharmacy, and Vendor Management Departments) routinely collects and reviews
documentation to verify that quality standards are met by clinical vendors who are delegated to
conduct utilization management on behalf of Plan members. In addition, an annual review of
each clinical vendor is completed by the Plan’s Clinical Vendor Oversight Committee to ensure
that each clinical vendor complies with delegated utilization management requirements,
including but not limited to contractual obligations and the guidelines specified in this section
of this policy related to the development, review, and application of objective, scientifically-
derived, and evidence-based clinical review criteria, with individual consideration of the
member’s status (when appropriate). If established quality standards are not met, the
delegated utilization management clinical vendor develops and implements a targeted and
measurable corrective action plan that is monitored by the Plan. For services managed by
clinical vendors with whom the Plan has delegated utilization management, the Plan evaluates
member access to treating facilities and availability of qualified providers (including care from
an out-of-network provider when clinically appropriate), member satisfaction, provider
satisfaction, member and provider timely access to applicable clinical review criteria, and the
vendor’s process for evaluating recommended revisions to clinical review criteria submitted by
actively practicing practitioners with appropriate credentials and clinical expertise.
Procedure
The Plan-adopted clinical review criteria are developed and implemented in accordance with generally
accepted standards of medical/clinical practice which are based on objective and credible scientific
evidence published in peer-reviewed medical literature generally recognized by the relevant medical
community, relying on controlled clinical trials. Practitioners with clinical expertise in the area being
reviewed have the opportunity to advise or comment on the development, adoption, and
implementation of all UM criteria utilized by the Plan; this includes feedback from qualified
Clinical Review Criteria
12 of 33
practitioners on staff at the Plan or delegated clinical vendors, outside physician consultants, provider
reviewers, participating providers in the Plan’s network, and practitioners treating Plan members.
See the Policy Summary and the Delegated Management sections of this policy for guidelines related
to applicable clinical review criteria and services managed by partner clinical vendors with whom the
Plan has delegated utilization management (by Plan product), including behavioral health services,
radiology services, pharmacy benefits administration, and durable medical equipment, prosthetics,
orthotics and supplies. Review the Clinical Technology Evaluation administrative policy, policy number
OCA 3.13, for a description of the Plan’s process for evaluating new technology and the new application
of existing technology.
1. Development and Review of the Plan’s Internal Clinical Review Criteria:
The Plan’s internal clinical review criteria are specified in the Plan’s medical policies or pharmacy
policies. Internal clinical review criteria are developed, reviewed at least annually, and updated as
necessary, utilizing the following resources (as applicable) to evaluate the clinical services,
treatments, and technologies for the specified indications and the application of medical necessity
criteria, as stated below in items a through l:
a. In consultation with the Plan’s Medical Director(s) and other Plan staff, as appropriate; AND
b. With input from actively practicing specialists and/or professionals or serving as consultants
who have expertise and appropriate credentials in the applicable clinical area under
consideration, as appropriate; e.g., criteria review by board-certified physician experts in the
Plan’s service area, feedback from participants of the local network-based Provider Advisory
Committee, and/or independent medical criteria review from board-certified physician
consultants from Advanced Medical Reviews (AMR). Consultants may include but are not
limited to pharmacists, community-based providers, behavioral health clinicians, dentists,
and/or board-certified physicians actively practicing in specialties that include neonatology,
pediatrics, family medicine, internal medicine, medical/surgical subspecialties, and/or geriatrics;
AND
c. In accordance with the Plan’s definition of medical necessity (as specified in the Medically
Necessary medical policy, policy number OCA 3.14), the Plan’s definition of experimental and
investigational services (as stated in the Experimental and Investigational Treatment medical
policy, policy number OCA 3.12), and the Plan’s definition of cosmetic and reconstructive or
restorative services (as documented in the Cosmetic, Reconstructive, and Restorative Services
medical policy, policy number OCA 3.69); AND
d. Review of unbiased, evidence-based assessments of health technologies, clinical programs,
and/or healthcare services to determine the impact of intervention(s) on patient safety and
clinical outcomes; AND

Clinical Review Criteria
13 of 33
e. Review of position papers and guidelines established or endorsed by nationally recognized
medical associations, specialty societies, dental organizations, or governmental agencies,
including but not limited to practice guidelines adopted by the Plan; AND
f. Clinical studies published in peer-reviewed scientific literature evaluating the use of the clinical
service as an alternative treatment strategy to established interventions considered the
standard of care for the specified indication (considering the patient’s medical condition, age,
comorbidities, and other factors applicable to the health outcomes of the clinical technology )
to determine if the service improves the net health outcome, is cost-effective compared to the
standard of care, and if the clinical outcomes outweigh any harmful effects; AND
g. The documented, favorable health outcomes are reasonably expected to be attainable outside
of the investigational settings (i.e., in a standard clinical setting) to a degree comparable in the
published, scientifically derived and evidence-based investigations; AND
h. When applicable, the clinical technology, including drugs, biologics, devices, or other products
requiring final approval to market, has final approval for the specified indication from the
appropriate governmental body(ies) with the authority to regulate the clinical technology (e.g.,
the U.S. Food and Drug Administration); AND
i. Policies, position statements, consensus reports, and standards adopted by governmental
agencies which may include but are not limited to the National Institutes of Health (NIH),
Agency for HealthCare Research and Quality (AHRQ), U.S. Center for Disease Control and
Prevention (CDC), Center for Medicare & Medicaid Services (CMS), Massachusetts Executive
Office of Health and Human Services, or New Hampshire Department of Health and Human
Services (e.g., U.S. Preventive Services Task Force, AAP Bright Futures); AND
j. Published scientific evidence from additional reputable sources concerning the safety and
effectiveness of the clinical treatment on health outcomes (i.e., proven benefit, unproven
benefit, insufficient evidence to determine effect, or documented harm) such as industry-
standard, evidence-based guidelines and recommendations (such as those established by
InterQual®, National Institute for Health and Care Excellences, National Comprehensive Cancer
Network); AND
k. Other sources deemed necessary to evaluate the clinical technology for the specified clinical
indication and to develop the Plan’s clinical coverage criteria; AND
l. With input from actively practicing practitioners with appropriate credentials and clinical
expertise in the applicable clinical area who have the opportunity to submit comments on
clinical review criteria utilized for Plan members (with feedback related to the development,
ongoing management, and/or application of those criteria). Practitioners may submit feedback
at any time through the Plan’s Provider Information Mailbox available at
Provider.Info@BMCHP-wellsense.org. The Plan will thoroughly research recommendations and
comments submitted from providers.

Clinical Review Criteria
14 of 33
On at least an annual basis, Plan staff review all clinical review criteria utilized by the Plan and
the procedures for applying those clinical review criteria; the Plan will evaluate provider
feedback submitted by practicing practitioners when evaluating applicable clinical review
criteria. If the practitioner would like to provide input on clinical review criteria that will be
considered during the internal policy’s next annual review, it is recommended that comments
and supporting references be submitted to the Plan a few months before the applicable policy’s
scheduled annual review date (as specified in the Next Review Date section at the end of each
internal policy). Supporting documentation must include position statements developed or
endorsed by nationally recognized professional associations, consensus reports or guidelines
from specialty societies, or standards adopted by governmental agencies (e.g., National
Institutes of Health, Agency for HealthCare Research and Quality, Center for Medicare &
Medicaid Services, Massachusetts Executive Office of Health and Human Services, or New
Hampshire Department of Health and Human Services). Published scientific evidence from
additional reputable sources may also be submitted for consideration.
Issues related to clinical review criteria that must be addressed before the policy’s annual
review date will be evaluated immediately during a prior authorization request for services; OCA
UM staff will engage in individual case discussions with licensed Plan pharmacists, OCA UM
clinicians, and/or Plan Medical Directors (utilizing qualified Plan clinicians applicable for the
member’s condition and requested treatment) to determine if the clinical review criteria are
appropriate for the member’s circumstances or care provided by a local delivery system
according to the guidelines specified below in the Application of the Plan’s Clinical Review
Criteria section of this policy.
Providers may email feedback on the Plan’s internal medical policies to the Medical Policy
Mailbox at medical.policy@bmchp-wellsense.org. It is important to include the medical policy
title and policy number with the comments so Plan staff can thoroughly research the issue. An
integral component of the Plan’s annual medical policy review process is to evaluate provider
comments and recommendations.
2. Application of Plan’s Internal Clinical Review Criteria and Plan-Adopted InterQual®
Criteria:
Review the Policy Summary and the Delegated Management sections (rather than this section of
the policy) for guidelines related to clinical review criteria and services managed by partner clinical
vendors with whom the Plan has delegated utilization management by Plan product. Application of
the Plan’s clinical review criteria (including internal clinical review criteria and InterQual® criteria)
follows the procedure specified below in items a through g:
a. The Plan’s Office of Clinical Affairs (OCA) includes OCA UM staff, Plan licensed pharmacists,
and Plan Medical Directors who apply applicable Plan clinical review criteria consistently when
determining the medical necessity of healthcare services. The Plan’s OCA UM staff includes
both the Pharmacy UM staff and UM staff. Reporting to the Director of Pharmacy, the
Clinical Review Criteria
15 of 33
Pharmacy UM staff reviews requests for pharmacotherapy or directs requests to a partner
clinical vendor for delegated utilization management. Reporting to the Directors of Utilization
Management, UM staff reviews medical/surgical/behavioral health requests for service or
directs requests to a partner clinical vendor for delegated utilization management according to
guidelines in both item (1) and item (2):
(1) The Plan’s OCA UM staff applies clinical review criteria consistently for all Plan members
according to the standards specified in this policy (e.g., requests for transplant services),
as well as complying with the Plan’s out-of-network guidelines and product-specific
requirements outlined in the Out-of-Network Services medical policy, policy number OCA
3.18. When standard clinical criteria are not met, qualified OCA UM staff also considers
member-specific factors impacting the member’s individual healthcare needs to
determine if the service is medically necessary for the requested indication. The service
may include a treatment, procedure, supply, device, biologic, or drug and will be used to
prevent, diagnose, stabilize, and/or treat a disease, condition, and/or disorder that results
in health impairment and/or disability, and/or the service allows the member to attain,
maintain, or regain functional capacity. Individual consideration includes an assessment of
any member-specific factors impacting care, including one or more of the following:
(a) Member’s condition;
(b) Member’s comorbidities;
(c) Member’s age, including the assessment of the member’s age-appropriate growth,
development, and competencies, as well as evaluation of age-related and condition-
specific healthcare needs and associated issues;
(d) Relevant past medical/surgical/behavioral health/dental/pharmacotherapy history;
(e) Complications;
(f) Progression of the member’s condition, illness, or injury;
(g) Diagnostic test results;
(h) Treatment outcomes;
(i) Treatment options;
(j) Psychosocial circumstances;
(k) Home and environmental factors impacting member’s clinical condition (e.g.,
homelessness, employment status, poverty, neighborhood);
Clinical Review Criteria
16 of 33
(l) Other healthcare services requested and/or provided to the member to integrate
healthcare for continuity, coordination, and collaboration of services;
(m) Local healthcare delivery system’s ability to meet the healthcare needs of the
member’s specific condition;
(n) Member’s reasonable accessibility to a qualified provider with appropriate
credentials, licensure, clinical expertise or resources in the applicable clinical area
necessary to adequately manage the member’s condition, including but not limited
to pharmacotherapy, behavioral health services, dental services, radiology services,
or durable medical equipment (prosthetics, orthotics and supplies);
(o) Other factors related to the member’s plan of care or health outcomes; AND/OR
(p) If applicable, verification that the requested device, system, biologic, or drug is being
prescribed/requested and will be utilized according to its FDA-approved or
compendia indication and guideline information, including intended use for the
member’s age and medical condition; AND
(2) When clinical review criteria are NOT met for a specified service such that medical
necessity cannot be established, OCA UM staff will engage in individual case discussions
with licensed Plan pharmacists, OCA UM clinicians, and/or Plan Medical Directors (utilizing
qualified Plan clinicians applicable for the member’s condition and requested treatment)
to determine if the clinical review criteria are appropriate for the member’s circumstances
or care provided by a local delivery system. If the clinical review criteria are not
appropriate, OCA UM staff may make the utilization determination based on the
member’s condition and other unique circumstances; AND
b. OCA UM staff considers the following characteristics of the healthcare delivery system listed in
items (1) through (4) to assess the local healthcare delivery system’s ability to meet the
member’s healthcare needs when applying clinical review criteria to each request:
(1) Availability and member access to acute and subacute care facilities, including but not
limited to acute care inpatient hospitals (with access to inpatient and outpatient specialty
hospital services such as major burn care, transplantation, specialty pediatric care,
specialty outpatient centers for HIV/AIDS, sickle cell disease, hemophilia, craniofacial and
congenital anomalies), surgi-centers, rehabilitation facilities, transitional care facilities,
skilled nursing facilities (SNF), home health agencies, and hospice programs, as applicable
for the member’s clinical needs; AND
(2) Member’s reasonable accessibility to a qualified provider with appropriate credentials and
clinical expertise in the applicable clinical area necessary to adequately treat the
member’s condition; AND
Clinical Review Criteria
17 of 33
Note: The Plan will authorize a member’s care from an out-of-network provider when, as
determined by the Plan, the care needed by the member is not available or is not
reasonably accessible to the member.
(3) Covered benefits for acute and subacute care facilities, including but not limited to acute
care inpatient hospitals, surgi-centers, rehabilitation facilities, transitional care facilities,
SNF, or home health agencies, as applicable for the member’s clinical needs; AND
(4) The ability of acute and subacute care facilities, including but not limited to acute care
inpatient hospitals, surgi-centers, rehabilitation facilities, transitional care facilities, SNF,
or home health agencies, to provide the following services, as specified below in BOTH
items (a) and (b):
(a) Provide the recommended medically necessary services to the member within the
estimated amount, frequency, and duration of treatment (including the estimated
length of stay, when applicable); medically necessary services required by the
member and provided by the facility/treating provider may include routine
medical/surgical services, highly specialized healthcare services (such as transplant
services or cancer care), rehabilitative care, habilitative services, and/or support
services after hospital discharge; AND
(b) Provide the medically necessary clinical support to the Plan member after the
member’s hospital discharge and/or transition to a less intense clinical setting or to
home, as applicable for the member’s treatment plan; AND
c. When an OCA UM staff member is unable to authorize care by establishing medical necessity,
the OCA UM staff will forward the request and documentation to the appropriate Medical
Director or licensed Plan pharmacist for a determination (utilizing qualified Plan clinicians
applicable for the member’s condition and requested treatment); AND
d. When medical necessity cannot be established through existing clinical review criteria, the
Plan’s Medical Directors and/or licensed Plan pharmacists consider alternate methods of
determining medical necessity, as defined in the Medically Necessary medical policy, policy
number OCA 3.14. If Plan-adopted written clinical review criteria have not been established for
the requested service for the specified indication, the Plan’s Medical Directors and/or licensed
Plan pharmacists will use published and applicable generally accepted, scientifically-based
standards of care to determine medical necessity. If scientifically-based standards of care are
not available, observational studies from more than one (1) institution that suggest a causal
relationship between the service or treatment and health outcomes may be used by the Plan’s
Medical Directors and/or licensed Plan pharmacists to make medical necessity determinations
if these observational studies are clinically appropriate with respect to the member’s clinical
presentation. The Plan’s Medical Directors and/or licensed Plan pharmacists also consider
member-specific factors when applying clinical criteria, evaluating standards of care and
credible scientific evidence published in peer-reviewed medical/clinical literature, and/or

Clinical Review Criteria
18 of 33
reviewing observational studies for a request for services for a Plan member to make medical
necessity determinations; AND
e. The Medical Policy, Criteria, and Technology Assessment Committee (MPCTAC), Pharmacy
and Therapeutics (P&T) Committee, Utilization Management Committee (UMC), and other
applicable committees meet annually or more frequently as needed to review and/or and
authorize all clinical review criteria used by the Plan along with the policies and procedures for
application; AND
f. OCA UM staff training and annual inter-rater reliability testing are conducted to review the
application of internal clinical review criteria (including criteria in the Plan’s internal medical
policies and internal pharmacy policies) and Plan-adopted InterQual® criteria to ensure the
consistency of medical necessity determinations among the OCA UM staff, Plan pharmacists,
and Plan Medical Directors (according to the definitions of inter-rater reliability, OCA Staff, and
OCA UM Staff in the Definitions section of this policy); AND
g. The Plan makes all of its clinical review criteria available to practitioners, members, regulatory
agencies, and accreditation organizations, upon oral or written request. Providers and member
may call or fax the Plan with a request for a copy of the specific criteria, as stated in writing in
the Plan‘s provider manual and Plan’s website. This access to clinical review criteria includes
applicable copyrighted commercial criteria such as those used by the Plan’s partner delegated
clinical vendors and Plan-adopted InterQual® criteria.
The current version of clinical review criteria included in the Plan’s internal medical policies and
internal pharmacy policies are available to all providers, members, and the general public on the
Plan’s extranet site. Participating providers receive network notifications via email at least 60
calendar days before the effective date of material changes to internal clinical review criteria
and/or coding (excluding industry-wide code updates and administrative changes) or when new
versions of InterQual® criteria are adopted by the Plan. Copies of internal medical policies with
material changes to clinical review criteria and/or coding are included these provider network
notifications (sent at least 60 calendar days before the effective date); updated internal
medical policies will be available at the Plan’s website on the effective date of the revisions.
Providers may email feedback on the Plan’s medical policies to the Medical Policy Mailbox at
medical.policy@bmchp-wellsense.org. It is important to include the medical policy title and
policy number with the comments so Plan staff can thoroughly research the issue. An integral
component of the Plan’s annual medical policy review process is to evaluate provider comments
and recommendations.
The Plan will submit material revisions to its medical necessity guidelines, including clinical
review criteria and related utilization management protocols, to the Massachusetts Office of
Patient Protection, Massachusetts Executive Office of Health and Human Services (EOHHS),
New Hampshire Department of Health and Human Services (DHHS), and the Centers for
Medicare & Medicaid Services (CMS) at least 60 calendar days before the effective date of
these material revisions (or another timeframe specified by the organization) when these
Clinical Review Criteria
19 of 33
changes may impact services provided to the organization’s enrollees; a designated contact
person must be provided in writing to the Medical Policy, Criteria, and Technology Assessment
Committee (MPCTAC) by the organization or its designee.
Internal pharmacy policy revisions are communicated to providers 60 calendar days before the
effective date of the revisions. Pharmacy policies for the Plan’s NH Medicaid product are
submitted to DHHS for review and approval prior to implementation. Once approved,
pharmacy policies are available on the Plan’s website 30 calendar days before the effective
date. For Medicaid and commercial lines of business, providers may email feedback on the
Plan’s pharmacy policies at pharma[email protected], or provide feedback as part of
the UM process during Peer to Peer discussions with the Plan’s clinical staff. During the annual
pharmacy policy review process, the Plan evaluates provider feedback and recommendations.
Pharmacy policies for Medicaid and commercial products are approved by the Plan’s Pharmacy
& Therapeutics (P&T) Committee. For MA Senior Care Options (SCO) and NH Medicare
Advantage products, the pharmacy policies are approved by the Centers for Medicare &
Medicaid Services. Pharmacy utilization management functions and the P&T Committee
responsibilities are delegated to the Pharmacy Benefit Manager for MA SCO and NH Medicare
Advantage products.
Responsibility and Accountability
See the Policy Summary and Delegated Management sections of this policy for guidelines related to
clinical review criteria and services managed by clinical vendors with whom the Plan has delegated
utilization management (by Plan product), including behavioral health services, radiology services,
dental services, pharmacy benefits administration, and durable medical equipment, prosthetics,
orthotics and supplies. Responsibility and accountability related to the development, implementation,
and monitoring of the Plan’s internal clinical review criteria (included in the Plan’s medical policies and
internal pharmacy policies) are specified below in items 1 through 4:
1. The Utilization Management Committee (UMC), chaired by the Director of UM Program
Oversight and Member Appeals and Grievances, oversees and is accountable for the adoption,
development, review, update, and implementation of the Plan’s clinical review criteria.
Generally, the Plan adopts nationally developed and accepted criteria (e.g., InterQual®). When
national criteria are not available or not utilized by the Plan, Plan-specific criteria may be
developed that are objective, scientifically derived, and evidence-based, with input from
participating practitioners and consistent with applicable legal, regulatory, and national
accreditation organization standards.
2. The Medical Policy, Criteria, and Technology Assessment Committee (MPCTAC) is responsible
for developing and approving medical policies, and the Pharmacy and Therapeutics (P&T)
Committee is responsible for developing and approving pharmaceutical coverage policies.
3. The Directors of OCA (including but not limited to the Directors of Utilization Management and
the Director of Pharmacy), Chief Medical Officer, Plan Medical Directors, Plan pharmacists, and
Clinical Review Criteria
20 of 33
other OCA UM staff use the Plan’s clinical review criteria in accordance with applicable Plan
policies and procedures.
4. The Directors of OCA, including but not limited to the Directors of Utilization Management and
the Director of Pharmacy, or their designee(s) are responsible for ensuring OCA UM staff
training, evaluating, and monitoring. The Chief Medical Officer or designee is responsible for
ensuring Medical Director training, evaluation, and monitoring to ensure consistent application
of clinical review criteria and medical necessity determinations.
Variations
The Plan uses guidance from the Centers for Medicare & Medicaid Services (CMS) for medical
necessity and coverage determinations for the Plan’s Senior Care Options (SCO) members and New
Hampshire Medicare Advantage HMO members, including but not limited to national coverage
determinations (NCDs), local coverage determinations (LCDs), local coverage articles (LCAs), and
documentation included in Medicare manuals. Verify CMS guidelines in effect on the date of the prior
authorization request. When there is no guidance from CMS for the requested service, Plan-adopted
clinical review criteria will be used to determine the medical necessity of the service.
Definitions
Clinical Review Criteria (Definition for MassHealth and Senior Care Options Products):
Criteria used to determine the most clinically appropriate and necessary level of care and intensity of
services to ensure the provision of medically necessary services. Medical necessity guidelines
established by the Plan will be no more restrictive than the applicable contractual MassHealth ACO and
MCO definition of Medically Necessary or Medical Necessity and the same services furnished to
members under MassHealth fee-for-service, as specified in the Plan’s Medically Necessary medical
policy, policy number OCA 3.14. Any new or amended pre-authorization requirement or restriction shall
NOT be implemented unless the Plan’s and/or partner clinical vendor’s respective website has been
updated to clearly reflect the new or amended requirement or restriction.
Clinical Review Criteria (Definition for Qualified Health Plans/ConnectorCare/Employer
Choice Direct Definition Products): In accordance with 958 CMR 3.020, clinical review criteria are
the written screening procedures, decisions, abstracts, clinical protocols and/or practice guidelines
used by the Plan to determine the medical necessity and appropriateness of health care services.
Utilization review criteria shall be up to date and applied consistently by the Plan or the Plan’s partner
clinical vendor and made easily accessible to members, providers, and the general public on the Plan’s
website; or, in the alternative, on the Plan’s partner clinical vendor’s website so long as the Plan
provides a link on its website to the vendor’s website; provided, however, that the Plan shall not be
required to disclose licensed, proprietary criteria purchased by the Plan or partner clinical vendor on its
website, but must disclose such criteria to a provider or subscriber upon request. Review the Plan’s
Medically Necessary medical policy, policy number OCA 3.14, for the product-specific definition of
medically necessary treatment. Any new or amended pre-authorization requirement or restriction shall
NOT be implemented unless the Plan’s and/or partner clinical vendor’s respective website has been
updated to clearly reflect the new or amended requirement or restriction.
Clinical Review Criteria
21 of 33
Clinical Review Criteria (Definition for New Hampshire Medicaid Product): A set of medical
decision standards employed in the utilization review process in order to ensure members receive
appropriate care, at an appropriate time, in an appropriate setting by an appropriate provider and at an
appropriate level of care. Criteria are consistent with an efficient and effective utilization of resources
available to recipients. Medical necessity guidelines established by the Plan will be no more restrictive
than the contractual definition of Medically Necessary for the New Hampshire Department of Health
and Human Services (DHHS) and the same services furnished in the New Hampshire DHHS fee-for-
service Medicaid program, as specified in the Plan’s Medically Necessary medical policy, policy number
OCA 3.14. Any new or amended pre-authorization requirement or restriction shall NOT be
implemented unless the Plan’s and/or partner clinical vendor’s respective website has been updated to
clearly reflect the new or amended requirement or restriction.
Inter-Rater Reliability (IRR): A performance measurement tool used to compare and evaluate the
level of consistency in healthcare determinations between two (2) or more medical and behavioral
health utilization management (UM) clinicians. The tool is used to minimize variation in the application
of clinical review criteria and identify potentially avoidable utilization target areas that need
improvement and evaluate the ability to identify quality of care issues.
Office of Clinical Affairs (OCA) Staff: Plan staff members within the OCA that include but are not
limited to OCA Utilization Management (UM) staff, Plan licensed pharmacists, Plan Medical Directors,
and the Chief Medical Officer. The Directors of OCA, including the Directors of Utilization
Management and the Director of Pharmacy, or their designees are responsible for ensuring OCA UM
staff training, evaluating, and monitoring. The Plan’s OCA UM staff, Plan licensed pharmacists, and
Plan Medical Directors consistently use applicable Plan clinical review criteria when determining the
medical necessity of healthcare services. The Chief Medical Officer or designee is responsible for
ensuring Medical Director training, evaluation, and monitoring to ensure consistent application of
clinical review criteria and medical necessity determinations.
Office of Clinical Affairs (OCA) Utilization Management (UM) Staff: The Plan’s OCA UM staff
includes both the Pharmacy UM staff and UM staff. Reporting to the Director of Pharmacy, the
Pharmacy UM staff reviews requests for pharmacotherapy or directs requests to a partner clinical
vendor for delegated utilization management. Reporting to the Directors of Utilization Management,
appropriately qualified UM staff reviews medical, surgical, behavioral health, and/or dental requests for
service or directs requests to a partner clinical vendor for delegated utilization management.
Plan-Adopted Clinical Review Criteria: Written clinical review criteria used to determine medical
necessity, including internally developed criteria specified in Plan medical policies and Plan pharmacy
policies, InterQual® criteria utilized by the Plan, and clinical guidelines established by delegated
management partners (for related services provided Plan members for applicable Plan products).
Practitioner (Definition for the Qualified Health Plans, ConnectorCare, and Employer Choice
Direct): A professional who provides healthcare services. Practitioners are usually required to be
licensed as defined by law.

Clinical Review Criteria
22 of 33
Utilization Review (UR): A set of formal techniques designed to monitor the use of, or evaluate the
clinical necessity, appropriateness, efficacy, or efficiency of, healthcare services, procedures, or
settings. Such techniques may include, but are not limited to, ambulatory review, prospective review,
second opinion, certification, concurrent review, case management, discharge planning, and/or
retrospective review.
References
American Society for Reproductive Medicine (ASRM). Practice Committee of ASRM. Definition of
experimental procedures: a committee opinion. Fertil Steril. 2013.
Centers for Medicare & Medicaid Services (CMS). EPSDT - A Guide for States: Coverage in the
Medicaid Benefit for Children and Adolescents. 2014 Jun.
Centers for Medicare & Medicaid Services (CMS). Manuals. Publication # 100-02. Medicare Benefit
Policy Manual.
Centers for Medicare & Medicaid Services (CMS). Manuals. Publication # 100-03. Medicare National
Coverage Determinations (NCD) Manual.
Centers for Medicare & Medicaid Services (CMS). Medicaid. Early and Periodic Screening, Diagnosis,
and Treatment. Medicaid.gov.
Centers for Medicare & Medicaid Services (CMS). Medicare Coverage Database (MCD).
Centers for Medicare & Medicaid Services (CMS). Transmittals.
Change Healthcare. InterQual® Overview.
Commonwealth of Massachusetts. Division of Insurance (DOI) Bulletins.
Commonwealth of Massachusetts. Mandatory Benefits Guide. Consumer Affairs and Business
Regulation.
Commonwealth of Massachusetts. MassHealth Provider Bulletins.
Commonwealth of Massachusetts. MassHealth Provider Manuals.
Commonwealth of Massachusetts. MassHealth Transmittal Letters.
Contract between the Commonwealth Health Insurance Connector Authority and Plan.

Clinical Review Criteria
23 of 33
Contract between the Executive Office of Health and Human Services (EOHHS) and the Plan to Serve
as an Accountable Care Partnership Plan for the Accountable Care Organization (ACO) Program.
Contract between the Massachusetts Executive Office of Health and Human Services (EOHHS) and
Plan.
Contract between the New Hampshire Department of Health and Human Services (DHHS) and Plan.
Hayes, a symplr Company.
Levenson JL. Psychological factors affecting other medical conditions: Clinical features, assessment,
and diagnosis. UpToDate. 2020 Nov 2.
Medicaid.gov. Early and Periodic Screening, Diagnostic, and Treatment. Centers for Medicare &
Medicaid Services.
National Committee for Quality Assurance (NCQA). HEDIS® & Performance Measurement.
National Committee for Quality Assurance (NCQA). Utilization Management Accreditation.
National Institute for Health and Care Excellence (NICE). NICE guidance.
New Hampshire Department of Health and Human Services. Billing Manuals.
New Hampshire Department of Health and Human Services. Provider Notices.
Senior Care Options Contract between the Massachusetts Executive Office of Health and Human
Services (EOHHS) and Plan and Medicare Advantage Special Needs Plan Contract between the
Centers for Medicare & Medicaid Services (CMS) and the Plan.
U. S. Food and Drug Administration (FDA). Device Labeling.
U. S. Food and Drug Administration (FDA). Drug Approvals and Databases.
U. S. Food and Drug Administration (FDA). Medical Device Databases.
Next Review Date
06/01/23
Authorizing Entity
MPCTAC

Clinical Review Criteria
24 of 33
Appendix
Appendix: Policy History
Other Applicable Policies
Administrative Policy - Clinical Technology Evaluation, policy number OCA 3.13
Administrative Policy - Inter Rater Reliability, policy number OCA 3.216
Administrative Policy - Mental Health Parity Administrative Policy - Assurance of Parity between Medical
and Behavioral Health Benefits, policy number BH1
Medical Policy - Clinical Trials, policy number OCA 3.192
Medical Policy - Cosmetic, Reconstructive, and Restorative Services, policy number OCA 3.69
Medical Policy - Experimental and Investigational Treatment, policy number OCA 3.12
Medical Policy - Medically Necessary, policy number OCA 3.14
Medical Policy - Out-of-Network Services, policy number OCA 3.18
Reimbursement Policy - Clinical Trials, policy number 4.134
Reimbursement Policy - Clinical Trials, policy number SCO 4.134
Reimbursement Policy - Clinical Trials, policy number WS 4.12
Reimbursement Policy - Early Intervention, policy number 4.3
Reimbursement Policy - Early and Periodic Screening, Diagnosis and Treatment (EPSDT), policy
number WS 4.15
Reimbursement Policy - General Billing and Coding Guidelines, policy number 4.31
Reimbursement Policy - General Billing and Coding Guidelines, policy number SCO 4.31
Reimbursement Policy - General Billing and Coding Guidelines, policy number WS 4.17
Reimbursement Policy - General Clinical Editing and Payment Accuracy Review Guidelines, policy
number 4.108
Reimbursement Policy - General Clinical Editing and Payment Accuracy Review Guidelines, policy
number SCO 4.108
Reimbursement Policy - General Clinical Editing and Payment Accuracy Review Guidelines, policy
number WS 4.18
Reimbursement Policy - Hospital, policy number WS 4.21
Reimbursement Policy - Inpatient Hospital, policy number 4.110
Reimbursement Policy - Inpatient Hospital, policy number SCO 4.110
Reimbursement Policy - Non-Participating Provider, policy number WS 4.5
Reimbursement Policy - Non-Reimbursed Codes, policy number 4.38
Reimbursement Policy - Non-Reimbursed Codes, policy number WS 4.38
Reimbursement Policy - Outpatient Hospital, policy number 4.17
Reimbursement Policy - Outpatient Hospital, policy number SCO 4.17
Reimbursement Policy - Physician and Non-Physician Practitioner Services, policy number 4.608
Reimbursement Policy - Physician and Non-Physician Practitioner Services, policy number SCO 4.608
Reimbursement Policy - Physician and Non-Physician Practitioner Services, policy number WS 4.28
Reimbursement Policy - Provider Preventable Conditions and Serious Reportable Events, policy number
4.610
Reimbursement Policy - Provider Preventable Conditions and Serious Reportable Events, policy number
SCO 4.610

Clinical Review Criteria
25 of 33
Reimbursement Policy - Provider Preventable Conditions and Serious Reportable Events, policy number
WS 4.29
Reference to Applicable Laws and Regulations
42 CFR 405.1060. Code of Federal Regulations. Applicability of National Coverage Determinations.
42 CFR 422.205. Code of Federal Regulations. Public Health, Centers for Medicare & Medicaid
Services. Medicare Advantage Program. Provider Antidiscrimination Rules.
42 CFR 438.100. Code of Federal Regulations. Public Health, Centers for Medicare & Medicaid
Services. Managed Care. Enrollee Rights and Protections. Enroll Rights.
42 CFR §438.210. Code of Federal Regulations. Public Health. Centers for Medicare & Medicaid
Services. Medical Assistance Programs. Managed Care. Coverage and Authorization of Services.
42 CFR Parts 438, 440, 456, and 457. Code of Federal Register. Vol. 81. No. 61. Medicaid and
Children's Health Insurance Programs; Mental Health Parity and Addiction Equity Act of 2008; the
Application of Mental Health Parity Requirements to Coverage Offered by Medicaid Managed Care
Organizations, the Children's Health Insurance Program (CHIP), and Alternative Benefit Plans.
Centers for Medicare & Medicaid Services (CMS). 2016 Mar 30.
42 CFR §440.210. Code of Federal Regulations. Public Health. Centers for Medicare & Medicaid
Services. Medical Assistance Programs. Medical Assistance Programs. Required Services for the
Categorically Needy.
42 CFR §441.56. Code of Federal Regulations. Public Health. Centers for Medicare & Medicaid
Services. Medical Assistance Programs. Medical Assistance Programs. Requirements and Limits
Applicable to Specific Services. Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) of
Individuals Under Age 21. Required Activities.
42 USC § 18001. United States Code. Patient Protection and Affordable Care Act. 2010.
42 USC § 18001. United States Code. Patient Protection and Affordable Care Act. 2010.
78 FR 48164-69. Federal Register. Centers for Medicare & Medicaid Services (CMS). Medicare
Program. Revised Process for Making National Coverage Determinations. 2013 Aug 7.
114.3 CMR 17.00. Code of Massachusetts Regulations. Division of Health Care Finance and Policy.
Medicine.
130 CMR. Code of Massachusetts Regulations. Division of Medical Assistance.
Clinical Review Criteria
26 of 33
130 CMR 410.00. Code of Massachusetts Regulations. Division of Medical Assistance. Outpatient
Hospital Services.
130 CMR 415.000. Code of Massachusetts Regulations. Division of Medical Assistance. Acute Inpatient
Hospital Services.
130 CMR 433.00. Code of Massachusetts Regulations. Division of Medical Assistance. Physician
Services.
130 CMR 440.00. Division of Medical Assistance. Code of Massachusetts Regulations. Early
Intervention Program Services.
130 CMR 450.000. Code of Massachusetts Regulations. Division of Medical Assistance. Administrative
and Billing Regulations.
130 CMR 450.117(J). Code of Massachusetts Regulations. Division of Medical Assistance. Administrative
and Billing Regulations. Managed Care Participation. Compliance with Mental Health Parity Law.
130 CMR 450.204. Code of Massachusetts Regulations. Division of Medical Assistance. Administrative
and Billing Regulations. Medically Necessary.
211 CMR 52.00. Code of Massachusetts Regulations. Division of Insurance. Managed Care Consumer
Protections and Accreditation of Carriers.
211 CMR 52.02. Code of Massachusetts Regulations. Division of Insurance. Managed Care Consumer
Protections and Accreditation of Carriers. Definitions. Clinical Review Criteria.
211 CMR 52.02. Code of Massachusetts Regulations. Division of Insurance. Managed Care Consumer
Protections and Accreditation of Carriers. Definitions. Medical Necessity or Medically Necessary.
211 CMR 52.02. Code of Massachusetts Regulations. Division of Insurance. Managed Care Consumer
Protections and Accreditation of Carriers. Definitions. Utilization Review.
958 CMR 3.020. Code of Massachusetts Regulations. Health Insurance Consumer Protection.
Definitions. Clinical Review Criteria.
958 CMR 3.020. Code of Massachusetts Regulations. Health Insurance Consumer Protection.
Definitions. Utilization Review.
958 CMR 3.020. Code of Massachusetts Regulations. Health Insurance Consumer Protection.
Definitions. Medical Necessity or Medically Necessary.
958 CMR 3.020. Code of Massachusetts Regulations. Health Insurance Consumer Protection.
Definitions. Utilization Review.
Clinical Review Criteria
27 of 33
958 CMR 3.101. Code of Massachusetts Regulations. Health Insurance Consumer Protection.
Definitions. Carrier’s Medical Necessity Guidelines.
958 CMR 3.400. Code of Massachusetts Regulations. Health Insurance Consumer Protection.
External Review.
Commonwealth of Massachusetts. Chapter 207 of the Acts of 2010 - An Act Relative to Insurance
Coverage for Autism.
Commonwealth of Massachusetts. Mandatory Benefits Guide. Consumer Affairs and Business
Regulation.
Commonwealth of Massachusetts. Massachusetts General Laws Mandating that Certain Health
Benefits Be Provided By Commercial Insurers, Blue Cross and Blue Shield and Health Maintenance
Organizations. Regulatory Citations. 2017 Oct 24.
Commonwealth of Massachusetts. MassHealth Provider Regulations.
He-W 500. New Hampshire Code of Administrative Rules. Medical Assistance.
He-W 530. New Hampshire Code of Administrative Rules. Medical Assistance. Service Limits, Co-
Payments, and Non-Covered Services.
He-W 530.01(e). New Hampshire Code of Administrative Rules. Medical Assistance. Service Limits,
Co-Payments, and Non-Covered Services. Definitions. Medically Necessary.
He-W 530.05(b)(4). New Hampshire Code of Administrative Rules. Medical Assistance. Non-Covered
Services. Experimental or Investigational Procedures.
He-W 531. New Hampshire Code of Administrative Rules. Medical Assistance. Physician Services.
He-W 531.01(a). New Hampshire Code of Administrative Rules. Medical Assistance. Physician Services.
Cosmetic Purpose.
He-W 543. New Hampshire Code of Administrative Rules. Medical Assistance. Hospital Services.
He-W 546. New Hampshire Code of Administrative Rules. Medical Assistance. Early and Periodic
Screening, Diagnosis and Treatment Service.
MGL c 233. Massachusetts General Laws. An Act Relative to HIV-Associated Lipodystrophy Syndrome
Treatment.
MGL c 1760. Massachusetts General Laws. Health Insurance Consumer Protections.
Clinical Review Criteria
28 of 33
The Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA). The Center for Consumer
Information & Insurance Oversight. Centers for Medicare and Medicaid Services (CMS).
Newborns’ and Mothers Health Protection Act of 1996 (NMHPA). The Center for Consumer
Information & Insurance Oversight. Centers for Medicare and Medicaid Services (CMS).
New Hampshire Department of Health and Human Services (DHHS). Certified Administrative Rules.
RSA 417-D:2-b. New Hampshire Revised Statutes Annotated. Women’s Health Care. Reconstructive
Surgery.
RSA Chapter 420-E. New Hampshire Revised Statutes. Insurance. Licensure of Medical Utilization
Review Entitles.
Social Security Act. Title XIX. 1902(a)(43), 1905(a)(4)(B), 1905(r). Grants to States for Medical
Assistance Programs. Early and Periodic Screening, Diagnosis, and Treatment (EPSDT).
Social Security Act. Title XXI. State Children’s Health Insurance Program.
U.S. Women's Health and Cancer Right Act of 1998.
Disclaimer Information:
Plan refers to Boston Medical Center Health Plan, Inc. which operates under the trade name WellSense Health Plan. Medical
Policies are the Plan’s guidelines for determining the medical necessity of certain services or supplies for purposes of
determining coverage. These Policies may also describe when a service or supply is considered experimental or
investigational, or cosmetic. In making coverage decisions, the Plan uses these guidelines and other Plan Policies, as well as
the Member’s benefit document, and when appropriate, coordinates with the Member’s health care Providers to consider the
individual Member’s health care needs.
Plan Policies are developed in accordance with applicable state and federal laws and regulations, and accrediting organization
standards (including NCQA). Medical Policies are also developed, as appropriate, with consideration of the medical necessity
definitions in various Plan products, review of current literature, consultation with practicing Providers in the Plan’s service
area who are medical experts in the particular field, and adherence to FDA and other government agency policies. Applicable
state or federal mandates, as well as the Member’s benefit document, take precedence over these guidelines. Policies are
reviewed and updated on an annual basis, or more frequently as needed. Treating providers are solely responsible for the
medical advice and treatment of Members.
The use of this Policy is neither a guarantee of payment nor a final prediction of how a specific claim(s) will be adjudicated.
Reimbursement is based on many factors, including member eligibility and benefits on the date of service; medical necessity;
utilization management guidelines (when applicable); coordination of benefits; adherence with applicable Plan policies and
procedures; clinical coding criteria; claim editing logic; and the applicable Plan – Provider agreement.
Clinical Review Criteria
29 of 33
Appendix: Policy History
Original
Approval Date
Original Effective
Date* and Version
Policy Owner
Original Policy
Approved by
Regulatory Approval:
08/01/08
MH Review: 02/19/10
Internal Approval:
07/24/07 and 08/13/07
08/13/07
Version 1
Director of Medical Policy as
Chair of Medical Policy,
Criteria, and Technology
Assessment Committee
(MPCTAC)
Utilization
Management
Committee (UMC)
*Effective date for MA QHP commercial product: 01/01/12.
*Effective date for New Hampshire Medicaid product: 01/01/13.
*Effective date for MA Senior Care Options product: 01/01/16.
*Effective date for New Hampshire Medicare Advantage HMO product: 01/01/22.
Note: Policy title was Clinical Criteria until 07/31/17. Policy title changed to Clinical Review Criteria as of
08/01/17.
Policy Revisions History
Review Date
Summary of Revisions
Revision Effective
Date and Version
Number
Approved by
04/22/08
Typos and formatting corrected. Removed
bullet stating Chief Medical Officer conducts
review on all criteria annually.
Version 2
04/22/08: UMC
05/07/08
Added authority for plan pharmacists to
render pharmacy denials.
Version 3
05/20/08: UMC
06/19/08: Quality
Improvement
Committee (QIC)
08/20/09
Changed titles within Health Services, minor
typos and formatting, updated references,
changed definition for clinical criteria.
Version 4
09/22/09: UMC
09/23/09: QIC
07/21/10
Updated names, departments and references,
extra definition for medically necessary was
removed.
Version 5
07/21/10: MPCTAC
08/25/10: QIC
07/01/11
Added medically necessary definition and
language for Commercial product.
Version 6
07/22/11: MPCTAC
08/24/11: QIC
07/01/12
References updated, moved Purpose section
of policy to the beginning of the document
and added reference for the Plan’s Prior
Authorization/ Notification Requirements
matrix. Referenced the Plan’s Medically
Necessary policy for a definition of medically
necessary for each member type and deleted
Version 7
07/18/12: MPCTAC
08/15/12: MPCTAC
Clinical Review Criteria
30 of 33
medically necessary definitions from this
policy. Added language regarding delegated
management in Policy Statement section.
Added reference to Physician Reviewers in
policy. Changed definition title from “Clinical
Criteria” to “Clinical Review Criteria.”
08/15/12
Off cycle review for New Hampshire Medicaid
product. Revised the Purpose, Definitions,
Policy Statement, reformatted Procedure,
updated references for all Plan products.
Version 8
08/17/12: MPCTAC
09/13/12: QIC
9/01/12
Added language to clarify the Plan’s UR
process that includes the evaluation of
member’s circumstances and local delivery
system, when clinically appropriate.
Version 9
09/19/12: MPCTAC
09/26/12: QIC
06/01/13
Review for effective date 07/18/13. Revised
title of chair for the Utilization Management
Committee.
07/18/13
Version 10
06/19/13: MPCTAC
07/18/13: QIC
06/01/14
Review for effective date 10/01/14. Updated
Purpose, Policy Statement, Delegated
Management, Procedure, Responsibility and
Accountability, Definitions, and References
sections.
10/01/14
Version 11
06/09/14: MPCTAC
07/09/14: QIC
06/01/15
Review for effective date 07/08/15.
Removed Commonwealth Care,
Commonwealth Choice, and Employer Choice
from the list of applicable products because
the products are no longer available.
Administrative changes made to Purpose,
Policy Statement, Delegated Management,
and Procedure sections.
07/08/15
Version 12
06/17/15: MPCTAC
07/08/15: QIC
09/01/15
Review for effective date 10/14/15. Added
reference to eviCore healthcare in the
Delegated Management section. Updated list
of applicable products, including the removal
of Common-wealth Care, Commonwealth
Choice, and Employer Choice because the
products are no longer available.
10/14/15
Version 13
09/16/15: MPCTAC
10/14/15: QIC
06/01/16
Review for effective date 07/13/16. Updated
with administrative changes to the Delegated
Management, References, and References to
Applicable Laws and Regulations sections.
07/13/16
Version 14
06/15/16: MPCTAC
07/13/16: QIC
05/01/17
Review for effective date 06/01/17.
Administrative changes made to the policy
title and the Purpose, Policy Statement,
Responsibility and Accountability, Definitions,
References, and Reference to Applicable
Laws and Regulations sections to clarify the
Plan’s clinical criteria review process and the
06/01/17
Version 15
05/17/17: MPCTAC
Clinical Review Criteria
31 of 33
use of these clinical criteria in utilization
review activities.
08/31/17
Updated the definition of Clinical Review
Criteria (for Massachusetts products) to
include requirements for the medical
necessity guidelines applicable for the
Accountable Care Organization (ACO).
Updated Product Applicability and Reference
sections to incorporate ACO.
08/31/17
Version 16
08/31/17: MPCTAC
(electronic vote)
06/01/18
Review for effective date 07/01/18.
Administrative changes made to the Policy
Statement, Procedure, Responsibility and
Accountability, References, Other Applicable
Policies, and Reference to Applicable Laws
and Regulations sections.
07/01/18
Version 17
06/20/18: MPCTAC
09/01/18
Review for effective date 12/01/18.
Administrative changes made to the Purpose
and Policy Summary sections. Updated
criteria in the Procedure section (clarifying
the existing process).
12/01/18
Version 18
09/19/18: MPCTAC
11/01/18
Review for effective date 12/01/18.
Administrative changes made to the Policy
Statement, Delegated Management, and
Procedure sections to clarify the existing
process available for practitioners to submit
comments related to clinical review criteria.
12/01/18
Version 19
11/21/18: MPCTAC
06/01/19
Review for effective date 07/01/19.
Administrative changes made to the Policy
Summary (formerly Purpose section), Policy
Statement, Delegated Management,
Procedure, Definitions, Responsibility and
Accountability, References, and Reference to
Applicable Laws and Regulations sections to
clarify the existing process.
07/01/19
Version 20
06/19/19: MPCTAC
12/01/19
Review for effective date 01/01/20.
Administrative changes made to the
Delegated Management and Procedure
sections.
01/01/20
Version 21
12/18/19: MPCTAC
06/01/20
Review for effective date 07/01/20.
Administrative changes made to the Policy
Summary, Procedure, References, and
Reference to Applicable Laws and
Regulations sections.
07/01/20
Version 22
06/17/20: MPCTAC
12/01/20
Review for effective date 01/01/21.
Administrative changes made to the
Delegated Management, Responsibility and
Accountability, and Definitions sections.
01/01/21
Version 23
12/16/20: MPCTAC
Clinical Review Criteria
32 of 33
12/22/20
Review for effective date 01/01/21 (replacing
version 23). Updated documentation related
to the Plan’s Pharmacy Manager, Express
Scripts, in the Delegated Management
section.
01/01/21
Version 24
12/23/20: MPCTAC
(electronic vote)
06/01/21
Review for effective date 07/01/21. Clarified
current guidelines with administrative
changes made to the Policy Summary, Policy
Statement, Delegated Management, and
Procedure sections to clarify existing
guidelines. Updated References section.
07/01/21
Version 25
06/16/21: MPCTAC
08/01/21
Review for effective date 09/01/21.
Administrative changes made to the Policy
Summary, Policy Statement, Definitions,
References, Other Applicable Policies, and
Reference to Applicable Laws and
Regulations sections to clarify current
guidelines.
09/01/21
Version 26
08/13/21: MPCTAC
(electronic vote)
11/01/21
Review for effective date 12/01/21. Added NH
Medicare Advantage HMO as an applicable
product effective 01/01/22. Administrative
changes made to the Policy Summary and
Policy Statement sections. Added the
Variations section.
12/01/21
Version 27
11/17/21: MPCTAC
07/01/22
Review for effective date 08/01/22.
Administrative changes made to the Policy
Summary, Policy Statement, Delegated
Management, Procedure, Responsibility and
Accountability, Definitions, and Other
Applicable Policies sections.
08/0/122
Version 28
07/25/22: MPCTAC
(electronic vote)
08/01/22
Review for effective date 11/01/22. Revised
the list of the Plan’s delegated services and
partner clinical vendors in the Delegated
Management section. eviCore healthcare
served as the Plan’s delegated vendor for
radiology services from 03/15/20 to 10/31/22.
Effective 11/01/22, the Plan will delegate the
management of radiology services,
musculoskeletal services (i.e., spine surgeries,
joint surgeries, and interventional pain
management treatments), genetic testing,
and outpatient rehabilitation services (i.e.,
physical therapy, occupational therapy, and
speech therapy after the initial evaluation) to
AIM Specialty Health.
11/01/22
Version 29
Version 29 NOT
implemented and
replaced with
Version 30 as of
11/01/22
08/26/22: MPCTAC
(electronic vote)
09/01/22
Review for effective date 11/01/22. Revised
the effective date of AIM’s management of
outpatient rehabilitation services from
11/01/22
Version 30
09/23/22: MPCTAC
(electronic vote)
Clinical Review Criteria
33 of 33
11/01/22 to 12/01/22 in the Delegated
Management section. All other policy
revisions approved for Version 29 are
implemented in Version 30 as of 11/01/22.
Policy added to the Other Applicable Policies
section.
Complementary and Alternative Medicine
1 of 10
Medical Policy
Complementary and Alternative Medicine
Policy Number: OCA 3.194
Version Number: 22
Version Effective Date: 12/01/22
Impacted Products
☐ All Products
☐ NH Medicaid
☒ NH Medicare Advantage
☒ MA MassHealth ACO
☒ MA MassHealth MCO
☐ MA Qualified Health Plans/Employer Choice Direct
☒ MA Senior Care Options
Note: Disclaimer and audit information is located at the end of this document.
Policy Summary
The Plan considers complementary and alternative medicine (CAM) NOT medically necessary unless
the service (including indication for treatment) is covered for the member. Prior authorization from
AIM Specialty Health is required for outpatient rehabilitation services.
Clinical Criteria
The member’s product-specific benefit documents will determine coverage for CAM services, as
specified below in items 1 and 2:
1. The Plan considers CAM services NOT medically necessary for Plan members, except as
covered in the member’s applicable benefit documents.
2. There may be separate medical policies that address the treatment of specific conditions or
procedures that supersede this policy. See the Plan’s Prior Authorization/Notification
Requirements matrix available at the Plan’s website for prior authorization guidelines by service
type.
Complementary and Alternative Medicine
2 of 10
Limitations and Exclusions
The Plan considers CAM to NOT be medically necessary due to insufficient scientific evidence
demonstrating the clinical validity and clinical utility of treatment unless the service (including
indication for treatment) is covered for the member. CAM include but are not limited to any of the
following services:
1. Whole medicine systems (e.g., homeopathic and naturopathic medicine, traditional Chinese
medicine such as Ayurveda).
2. Mind body medicine to improve the mind's ability to affect bodily function and symptoms (e.g.,
biofeedback except for treatment of urinary incontinence, hypnotherapy/hypnosis, meditation,
prayer, mental healing, therapies that use creative outlets such as art, music, or dance).
3. Substances found in nature (e.g., herbal products, vitamins, dietary supplements).
4. Manipulative and body based practices (e.g., massage, myotherapy, craniosacral therapy,
osteopathic manipulation, hippotherapy, yoga, reflexology).
5. Energy medicine (e.g., Reiki, therapeutic touch, pulsed fields, magnetic fields, electromagnetic,
or alternating-current or direct-current field).
Variations
The Plan uses guidance from the Centers for Medicare & Medicaid Services (CMS) for medical
necessity and coverage determinations for Senior Care Options (SCO) members and NH Medicare
Advantage HMO members, including but not limited to national coverage determinations (NCDs), local
coverage determinations (LCDs), local coverage articles (LCAs), and documentation included in
Medicare manuals. At the time of the Plan’s most recent policy review, there was no applicable clinical
policies by CMS. Verify CMS guidelines in effect on the date of the prior authorization request for the
service and indication for treatment. When there is no guidance from CMS for the requested service,
plan-adopted clinical review criteria will be used to determine the medical necessity of the service.
Applicable Coding
The Plan utilizes up-to-date, industry-standard Current Procedural Terminology (CPT) codes, Health
Care Common Procedure Coding System (HCPCS) codes, and International Statistical Classification
of Diseases and Related Health Problems, 10th revision (ICD-10) diagnosis codes in the Plan’s medical
policies. Since these codes may be updated at different intervals than the medical policy review cycle,
the list of applicable codes included in a policy is informational only and may not be all
inclusive. Applicable codes are subject to change without prior notification and do not guarantee
member coverage or provider reimbursement. Review the Plan’s reimbursement policies for Plan
billing guidelines. Providers are responsible for obtaining prior authorization for the services specified
in the Clinical Criteria section and Limitations and Exclusions section of a medical policy, even if an
Complementary and Alternative Medicine
3 of 10
applicable code appropriately describing the service is not included in the policy’s Applicable Coding
section. Providers are expected to report all services using the most up-to-date, industry-standard
procedures and diagnosis codes at the time of the service.
CPT/HCPCS Codes
Description: Service is considered NOT medically necessary, except as
specified in the member’s applicable benefit document
90880
Hypnotherapy
Plan note: Code is NOT payable for the Senior Care Options product.
M0075
Cellular therapy
Plan note: Code is NOT payable for the Senior Care Options and NH Medicare
Advantage HMO products.
References
American Chronic Pain Association (ACPA). ACPA Resource Guide to Chronic Pain management, An
Integrated Guide to Medical, Interventional, Behavioral Pharmacologic and Rehabilitation Therapies.
Feinberg S (ed.) American Chronic Pain Association Inc., Rocklin, California. 2019.
American College of Chest Physicians (ACCP). Deng GE, Rausch SM, Jones LW, Gulati A, Kumar NB,
Greenlee H, Pietanza MC, Cassileth BR. Complementary therapies and integrative medicine in lung
cancer: diagnosis and management of lung cancer, 3rd ed: ACCP evidence-based clinical practice
guidelines. Chest. 2013 May;143(5 Suppl):e420S-36S. doi: 10.1378/chest.12-2364. PMID: 23649450.
American College of Physicians (ACP). Qaseem A, Wilt TJ, McLean RM, Forciea MA; Clinical Guidelines
Committee of the American College of Physicians. Noninvasive Treatments for Acute, Subacute and
Chronic Low Back Pain: A Clinical Guideline from the ACP. Ann Intern Med. 2017 Apr 4;166(7):514-30.
doi: 10.7326/M16-2367. Epub 2017 Feb 14. PMID: 28192789.
American Society of Anesthesiologists (ASA), American Society of Regional Anesthesia and Pain
Medicine (ASRA). Rosenquist RW, Benzon HT, Connis RT, De Leon-Casasola OA, Glass D, Korevaar
WC, Cynwyd B, Mekhail NA, Merrill DG, NIckinovich DG, Rathnmell JP, Nai-Mei Sang C, Simon DL; ASA
Task Force on Chronic Pain Management. Practice guidelines for chronic pain management: an
updated report by the ASA Task Force on Chronic Pain Management and the ASRA. Anesthesiology.
2010 Apr;112(4):810-33. doi: 10.1097/ALN.0b013e3181c43103. PMID: 20124882.
Centers for Medicare & Medicaid Services (CMS). Manuals. Publication # 100-02. Medicare Benefit
Policy Manual.
Centers for Medicare & Medicaid Services (CMS). Manuals. Publication # 100-03. Medicare National
Coverage Determinations (NCD) Manual.
Complementary and Alternative Medicine
4 of 10
Centers for Medicare & Medicaid Services (CMS). Medicare Coverage Database (MCD).
Centers for Medicare & Medicaid Services (CMS). Transmittals.
Chou R, Deyo R, Friedly J, Skelly A, Hashimoto R, Weimer M, Fu R, Dana T, Kraegel P, Griffin J, Grusing
S, Brodt E. Noninvasive Treatments for Low Back Pain. Comparative Effectiveness Review No. 169.
(Prepared by the Pacific Northwest Evidence-based Practice Center under Contract No. 290-2012-
00014-I.) AHRQ Publication No. 16-EHC004-EF. Rockville, MD: Agency for Healthcare Research and
Quality. 2016 Feb.
Chou R, Deyo R, Friedly J, Skelly A, Hashimoto R, Weimer M, Fu R, Dana T, Kraegel P, Griffin J, Grusing
S, Brodt ED. Nonpharmacologic Therapies for Low Back Pain: A Systematic Review for an American
College of Physicians Clinical Practice Guideline. Ann Intern Med. 2017 Apr 4;166(7):493-505. doi:
10.7326/M16-2459. Epub 2017 Feb 14. PMID: 28192793.
Commonwealth of Massachusetts. Division of Insurance (DOI) Bulletins.
Commonwealth of Massachusetts. MassHealth Provider Bulletins.
Commonwealth of Massachusetts. MassHealth Provider Manuals.
Commonwealth of Massachusetts. MassHealth Transmittal Letters.
Greenlee H, Balneaves LG, Carlson LE, Cohen M, Deng G, Hershman D, Mumber M, Perlmutter J,
Seely D, Sen A, Zick SM, Tripathy D; Society for Integrative Oncology. Clinical practice guidelines on
the use of integrative therapies as supportive care in patients treated for breast cancer. J Natl Cancer
Inst Monogr. 2014 Nov;2014(50):346-58. doi: 10.1093/jnci monographs/lgu041. Review. Erratum in: J
Natl Cancer Inst Monogr. 2015 May;2015(51):98. PMID: 25749602.
Institute for Clinical Systems Improvement (ICSI). Pain: Assessment, Non-Opioid Treatment
Approaches and Opioid Management. Eighth Edition. Version 2. 2017 Aug.
Levy SE, Hyman SL. Complementary and alternative medicine treatments for children with autism
spectrum disorders. Child Adolesc Psychiatr Clin N Am. 2015 Jan;24(1):117-43. doi:
10.1016/j.chc.2014.09.004. Epub 2014 Oct 3. PMID: 25455579.
National Academies of Sciences, Engineering, and Medicine. 2017. Pain management and the opioid
epidemic: Balancing societal and individual benefits and risks of prescription opioid use. 2017 Jul 13.
Washington, DC: The National Academies Press. doi: https://doi.org/10.17226/24781.
National Cancer Institute. National Institutes of Health (NIH). Complementary and Alternative
Medicine. 2019 Sep 30.
Complementary and Alternative Medicine
5 of 10
National Center for Complementary and Integrative Health (NCCIH). National Institutes of Health
(NIH). Acupuncture. 2017 Sep 24.
National Center for Complementary and Integrative Health (NCCIH). National Institutes of Health
(NIH). Acupuncture: In Depth. 2017 Feb 21.
National Center for Complementary and Integrative Health (NCCIH). National Institutes of Health
(NIH). Complementary, Alternative, or Integrative Health: What’s In a Name? 2019 Apr 2.
New Hampshire Department of Health and Human Services. Billing Manuals.
New Hampshire Department of Health and Human Services. Provider Notices.
Office of Patient Centered Care and Cultural Transformation (OPCC&CT). Complementary and
Integrative Health (CIH) Resource Guide. Version 2. Last Update: 2017 Oct.
U.S. Department of Veterans Affairs (VA), Department of Defense (DoD). VA/DoD Clinical Practice
Guideline for Diagnosis and Treatment of Low Back Pain. Version 2.0 – 2017.
U.S. Department of Veterans Affairs. Department of Defense (DoD). VA/DoD Clinical Practice
Guideline for the Management of Chronic Multisymptom Illness CMI 2014.
U.S. National Library of Medicine. National Institutes of Health. Collection Development Manual.
Complementary and Alternative Medicine. 2018 Mar 26.
Yuan QL, Guo TM, Liu L, Sun F, Zhang YG. Traditional Chinese medicine for neck pain and low back
pain: a systematic review and meta-analysis. PLoS One. 2015 Feb 24;10(2):e0117146. doi:
10.1371/journal.pone.0117146. eCollection 2015. PMID: 25710765.
Next Review Date
02/01/23
Authorizing Entity
MPCTAC
Appendix
Appendix: Policy History
Disclaimer Information:
Plan refers to Boston Medical Center Health Plan, Inc. which operates under the trade name WellSense Health Plan. Medical
Policies are the Plan’s guidelines for determining the medical necessity of certain services or supplies for purposes of
determining coverage. These Policies may also describe when a service or supply is considered experimental or
Complementary and Alternative Medicine
6 of 10
investigational, or cosmetic. In making coverage decisions, the Plan uses these guidelines and other Plan Policies, as well as
the Member’s benefit document, and when appropriate, coordinates with the Member’s health care Providers to consider the
individual Member’s health care needs.
Plan Policies are developed in accordance with applicable state and federal laws and regulations, and accrediting organization
standards (including NCQA). Medical Policies are also developed, as appropriate, with consideration of the medical necessity
definitions in various Plan products, review of current literature, consultation with practicing Providers in the Plan’s service
area who are medical experts in the particular field, and adherence to FDA and other government agency policies. Applicable
state or federal mandates, as well as the Member’s benefit document, take precedence over these guidelines. Policies are
reviewed and updated on an annual basis, or more frequently as needed. Treating providers are solely responsible for the
medical advice and treatment of Members.
The use of this Policy is neither a guarantee of payment nor a final prediction of how a specific claim(s) will be adjudicated.
Reimbursement is based on many factors, including member eligibility and benefits on the date of service; medical necessity;
utilization management guidelines (when applicable); coordination of benefits; adherence with applicable Plan policies and
procedures; clinical coding criteria; claim editing logic; and the applicable Plan – Provider agreement.
Complementary and Alternative Medicine
7 of 10
Appendix: Policy History
Original
Approval Date
Original Effective
Date* and Version
Policy Owner
Original Policy
Approved by
Regulatory Approval: N/A
Internal Approval:
07/28/09: Medical Policy, Criteria, and
Technology Assessment Committee
(MPCTAC)
08/26/09: Quality Improvement
Committee (QIC)
11/01/09
Version 1
Director of
Medical Policy as
Chair of
MPCTAC
MPCTAC and QIC
*Effective Date for QHP Commercial Product: 01/01/12
*Effective Date for Senior Care Options Product: 01/01/16
*Effective Date for NH Medicare Advantage HMO Product: 01/01/22
Policy title was Complementary and Alternative Medicine, Including Acupuncture Treatment until 06/30/19. As of
07/01/19, policy title changed to Complementary and Alternative Medicine, Including Acupuncture. As of
01/01/22, policy title changed to Complementary and Alternative Medicine.
Policy Revisions History
Review
Date
Summary of Revisions
Revision Effective
Date and Version
Number
Approved by
07/01/10
Removed osteopathic manipulation from the list
of CAM services. Changed the “non-covered”
language to “not medically necessary,” added
massage by a massage therapist and updated
references.
Version 2
07/21/10: MPCTAC
08/25/10: QIC
07/01/11
Updated references and added commercial
language.
Version 3
07/22/11: MPCTAC
08/24/11: QIC
07/01/12
Updated references, added language to
Applicable Code section and added applicable
code list. Updated Summary section and
Applicable Code section to specify that
acupuncture is considered a medically necessary
service for Commonwealth Care and
MassHealth members when used for substance
abuse detoxification, as managed and
authorized by Beacon Health Strategies.
Included statement that acupuncture is not a
covered service for Commercial members and
Version 4
07/18/12: MPCTAC
08/22/12: QIC
Complementary and Alternative Medicine
8 of 10
added a reference to the Medically Necessary
policy in the Summary section.
05/01/13
Review for effective date 09/01/13. Updated
Summary section and applicable code list.
Referenced Reimbursement Guidelines:
Chiropractic Services (Spinal Manipulation),
policy number 4.114. Medical Policy Statement
section revised without changing criteria.
Hippotherapy added to applicable code list, and
the reference to the Hippotherapy policy
deleted from Medical Policy Statement section
(since Hippotherapy policy will be retired
effective 09/01/13). Renumbered policy from
OCA: 3.193 to OCA: 3.194.
09/01/13
Version 5
05/15/13: MPCTAC
06/20/13: QIC
05/01/14
Review for effective date 07/01/14. Updated
Summary section. Added acupuncture services
in the Description of Item or Service and Clinical
Background Information sections. Revised
language in Medical Policy Statement section
and Limitations section without changing
criteria. Updated references. Revised policy
title.
07/01/14
Version 6
05/21/14: MPCTAC
06/11/14: QIC
01/01/15
Review for effective date 03/01/15. Updated
Medical Policy Statement section to clarify
guidelines without changing criteria. Updated
references.
03/01/15
Version 7
01/21/15: MPCTAC
02/11/15: QIC
04/01/15
Review for effective date 06/01/15. Removed
Commonwealth Care, Commonwealth Choice,
and Employer Choice from the list of applicable
products because the products are no longer
available. Administrative changes made to the
Applicable Coding section, but no changes
made to the code list. Updated Summary and
References sections.
06/01/15
Version 8
04/15/15: MPCTAC
05/13/15: QIC
11/25/15
Review for effective date 01/01/16. Updated
template with list of applicable products and
notes. Administrative changes made to the
Summary, Medical Policy Statement, and
Limitations section without revising criteria.
Revised language in the Applicable Coding
section.
01/01/16
Version 9
11/18/15: MPCTAC
11/25/15: MPCTAC
(electronic vote)
12/09/15: QIC
04/01/16
Review for effective date 06/01/16. Updated
the Clinical Background Information,
References, and Reference to Applicable Laws
and Regulations sections.
06/01/16
Version 10
04/20/16: MPCTAC
05/23/16: QIC
Complementary and Alternative Medicine
9 of 10
04/01/17
Review for effective date 05/08/17.
Administrative changes made to the Medical
Policy Statement and Applicable Coding
sections (without changing the code list or
criteria). Updated Definitions, Clinical
Background Information, References, and
Reference to Applicable Laws and Regulations
sections.
05/08/17
Version 11
04/19/17: MPCTAC
02/01/18
Review for effective date 03/01/18. Updated
Description of Item or Service and Other
Applicable Policies sections.
03/01/18
Version 12
02/21/18: MPCTAC
05/01/18
Review for effective date 06/01/18.
Administrative changes made to the Limitations
sections. Updated Plan notes in the Applicable
Coding section without changing the code list.
Removed QHP/ConnectorCare/Employer
Choice Direct from the list of applicable
products for this policy. Updated Policy
Summary, Definitions, References, and Other
Applicable Policies sections.
06/01/18
Version 13
05/16/18: MPCTAC
03/01/19
Review for effective date 04/01/19.
Administrative changes made to the Description
of Item or Service, Limitations, Applicable
Coding (with Plan notes added), References,
and Other Applicable Policies sections.
04/01/19
Version 14
03/20/19: MPCTAC
04/01/19
Review for effective date 05/01/19.
Administrative changes made to the Policy
Summary, Description of Item or Service,
Medical Policy Statement, and Limitations
sections. Revised the policy title. Removed
non-payable code listed as not medical
necessary (administrative change) and updated
Plan notes in the Applicable Coding section.
05/01/19
Version 15
04/18/19: MPCTAC
(electronic vote)
12/01/19
Review for effective date 01/01/20.
Administrative changes made to Plan notes in
the Applicable Coding section, References
section, and Reference to Applicable Laws and
Regulations section.
01/01/20
Version 16
12/18/19: MPCTAC
04/01/20
Review for effective date 07/01/20.
Administrative changes made to the Policy
Summary, Clinical Background Information,
References, and Reference to Applicable Laws
and Regulations sections. Revised the Plan
notes in the Applicable Coding section. Add a
prior authorization requirement for acupuncture
07/01/20
Version 17
04/15/20:
MPCTAC
Complementary and Alternative Medicine
10 of 10
for Senior Care Options members in the Medical
Policy Statement and Limitations sections.
12/01/20
Review for effective date 01/01/21.
Administrative changes made to the Description
of Item or Service, Medical Policy Statement,
Applicable Coding, and References sections.
01/01/21
Version 18
12/16/20: MPCTAC
11/01/21
Review for effective date 12/01/21. Adopted
new medical policy template; removed
administrative sections, the Medical Policy
Statement section renamed the Clinical Criteria
section, and the Limitations section renamed
the Limitations and Exclusions section. Added
NH Medicare Advantage HMO as an applicable
product effective 01/01/22. Administrative
changes made to the Policy Summary, Clinical
Criteria, Limitations and Exclusions, Applicable
Coding, and References sections.
01/01/22
Version 19
11/17/21: MPCTAC
12/01/21
Review for effective date 01/01/22. Removed
acupuncture references. Review the Plan’s
Acupuncture medical policy, policy number OCA
3.17, rather than this policy for acupuncture
services as of 01/01/22.
01/01/22
Version 20
12/15/21: MPCTAC
08/01/22
Review for effective date 11/01/22.
Administrative changes made to the Policy
Summary, Clinical Criteria, and Limitations and
Exclusions sections. Revised coding in the
Applicable Coding section.
11/01/22
Version 21
Version 21 NOT
implemented; Version
20 effective 01/01/22
to 11/30/22
08/26/22: MPCTAC
(electronic vote)
09/01/22
Review for effective date 12/01/22. The
effective date of AIM Specialty Health’s
management of outpatient rehabilitation
services changed from 11/01/22 to 12/01/22.
Administrative changes made to the Policy
Summary, Clinical Criteria, and Limitations and
Exclusions sections. Revised coding in the
Applicable Coding section.
12/01/22
Version 22
09/23/22: MPCTAC
(electronic vote)
Gender Affirmation Services
1 of 29
Medical Policy
Gender Affirmation Services
Policy Number: OCA 3.11
Version Number: 22
Version Effective Date: 12/01/22
Impacted Products
☒ All Products
☒ NH Medicaid
☒ NH Medicare Advantage
☒ MA MassHealth ACO
☒ MA MassHealth MCO
☒ MA Qualified Health Plans/Employer Choice Direct
☒ MA Senior Care Options
Note: Disclaimer and audit information is located at the end of this document.
Policy Summary
Gender affirmation surgeries and permanent hair removal require prior authorization and are
considered medically necessary for a member seeking treatment for gender dysphoria when Plan
medical criteria are met. Gender affirmation surgeries may include one (1) or more surgical procedures
and are part of a complex treatment plan involving medical, surgical, and behavioral health
interventions to achieve the desired outcomes for the individual.
Voice therapy is considered medically necessary as a treatment option for gender dysphoria when AIM
clinical appropriateness guidelines are met; prior authorization from AIM Specialty Health is required.
The Plan and the Plan’s delegated clinical vendors conducting utilization management do NOT
discriminate, arbitrarily deny, and/or impose stricter requirements by reducing the amount, duration,
and/or scope of required and medically necessary services for ANY Plan member based on the
member’s diagnosis, type of illness, health status or condition, sex, gender identity/gender dysphoria,
and/or sexual orientation. The full range of medical and/or surgical treatment options available to
individuals diagnosed with gender dysphoria may include, but are not limited to, those listed in
professional medical publications such as the current version of WPATH Standards of Care for Health
and Transsexual, Transgender and Gender-Nonconforming People.
Breast reconstruction used for the treatment of members with persistent, well-documented gender
dysphoria may include the medically necessary surgical removal of breast implants and/or the

Gender Affirmation Services
2 of 29
replacement of breast implants after implant explantation (including when the implant was initially
inserted as a component of a gender affirmation surgery); review the criteria in the Breast
Reconstruction medical policy, policy number OCA 3.43, rather than the criteria included in this policy.
Feminizing/masculinizing hormonal therapy and/or gender affirmation surgeries may limit the
member’s fertility. Infertility services are covered for some Plan products. Review the Plan’s Infertility
Services medical policy, policy number OCA 3.725.
Clinical Criteria
Applicable criteria must be met for gender affirmation services in item I for gender affirmation surgery
and permanent hair removal and/or item II for gender affirmation services that require Plan Medical
Director review.
I. The Plan considers gender affirmation services medically necessary for the treatment of gender
dysphoria, and Plan prior authorization is required for the services specified in this section. ALL
applicable Plan clinical review criteria must be met in items A through C:
A. Referral/Initial Assessment by Qualified Licensed Mental Health Professional:
There is a referral/initial assessment from a licensed qualified mental health professional that
contains ALL of the following documentation listed in items 1 through 8:
1. Gender identity resulting in a definitive diagnosis of persistent, well-documented gender
dysphoria (meeting DSM-5 criteria) for at least 6 months, history and development of
gender dysphoric feelings, and impact of stigma attached to gender nonconformity; AND
2. If living in an identity-congruent gender role, documentation of member’s experience, start
date, and if living full-time in identity-congruent gender role; AND
3. The member’s general identifying characteristics; AND
4. Results of psychosocial assessment, including any diagnoses and confirmation that other
behavioral health conditions are appropriately managed, reasonably controlled, and not
contributing to gender dysphoria); AND
5. Duration of mental health professional’s relationship with member, including type of
evaluation and therapy/counseling to date; AND
6. Written clinical rationale supporting member’s request for specific treatment(s); AND
7. Statement that mental health professional is available for coordination of care and plan of
care is in place; AND
8. Member’s psychological readiness for the requested treatment(s) with no contraindications
to treatment documented, including member’s capacity to make a fully informed decision
Gender Affirmation Services
3 of 29
and has the capacity to consent for treatment(s), and includes parental or guardian consent
(as applicable) if the member is younger than age 18 on the date of service unless the
adolescent member is emancipated at the time the service is rendered; AND
B. Member age 18 or older on the date of service; AND
C. Service-Specific Criteria:
Criteria must be met in item 1 for all gender affirmation surgical procedures and procedure
specific criteria must be met in item 2:
1. Gender Affirmation Surgical Procedures:
All criteria must be met in items a through e for any gender affirmation surgery:
a. Requests for prior authorization for each gender affirmation surgery must be submitted
by the surgeon (or the surgeon’s designee) performing the procedure and accompanied
by written clinical documentation; AND
b. Surgeon has reviewed the documentation by the qualified licensed mental health
professional (referenced above in item A), including the DSM-5 diagnosis of gender
dysphoria, and documentation from the member’s health care provider; AND
c. Surgeon has discussed risks and complications of proposed surgery and various surgical
techniques, surgeon’s own complication rates, impact on fertility, procedures for
preservation of fertility, and has obtained member’s informed consent; AND
d. If hormone therapy is a required criterion for a gender affirmation surgery (as specified
below in the procedure-specific criteria), medical records must document member
compliance with the prescribed regimen and clinical response over the course of
hormone therapy; AND
e. Member’s treating surgeon has documented that there are no contraindications to the
planned surgery, verified significant medical conditions are stable, and agrees with the
plan of care; AND
2. Procedure-Specific Criteria:
Procedure-specific criteria must be met for ANY procedure listed in items a through h:
a. Chest Procedures:
(1) Bilateral augmentation mammoplasty (with implantation of breast prostheses or
lipofilling) when the member has had 12 continuous months of clinician-supervised
Gender Affirmation Services
4 of 29
hormone therapy (unless hormone therapy is medically contraindicated for the
member), and the hormone therapy has not resulted in sufficient breast
development as self-reported by the member to the treating provider; OR
(2) Bilateral breast reduction, mastectomy, and/or chest reconstruction is requested;
OR
b. Feminizing Genital Surgery:
ALL guidelines must be met in items (1) through (4):
(1) ANY of the procedures in items (a) through (g) will be performed:
(a) Clitoroplasty/neoclitoroplasty;
(b) Labiaplasty/neolabiaplasty;
(c) Orchiectomy;
(d) Penectomy;
(e) Urethroplasty and urethra-meatoplasty;
(f) Vaginoplasty (also known as neovaginoplasty); e.g., penile inversion
vaginoplasty, colovaginoplasty, peritoneal pulldown vaginoplasty;
(g) Vulvoplasty/neovulvoplasty; AND
(2) Member has been assessed by 2 independently licensed health professionals, one
of whom must be a licensed qualified behavioral health professional (referenced
above in item A) and the other a clinician familiar with the member’s health, with
each assessment resulting in a diagnosis of gender dysphoria meeting DSM-5
criteria. The initial diagnosis (from one professional) must have been present for
at least 6 months; AND
(3) Member has had 12 continuous months of living as the gender that is congruent
with the member’s identity. Exceptions may be provided on a case-by-case basis
should the request for prior authorization document that compliance with this
requirement would jeopardize the health, safety, and/or well-being of the member;
AND
(4) The member has had 12 continuous months of clinician-supervised hormone
therapy appropriate to the member’s gender goals, unless hormone therapy is
medically contraindicated; OR
Gender Affirmation Services
5 of 29
c. Masculinizing Genital Surgery:
ALL guidelines must be met in items (1) through (4):
(1) ANY of the procedures listed in items (a) through (i) will be performed:
(a) Hysterectomy;
(b) Metoidioplasty;
(c) Oophorectomy;
(d) Phalloplasty with implantation of penile prosthesis;
(e) Salpingectomy;
(f) Scrotoplasty with insertion of testicular implants;
(g) Urethroplasty;
(h) Vaginectomy;
(i) Vulvectomy; AND
(2) Member has been assessed by 2 independently licensed health professionals, one
of whom must be a licensed qualified behavioral health professional (referenced
above in item A) and the other a clinician familiar with the member’s health, with
each assessment resulting in a diagnosis of gender dysphoria meeting DSM-5
criteria. The initial diagnosis (from 1 professional) must have been present for at
least 6 months; AND
(3) Member has had 12 continuous months of living as the gender that is congruent
with the member’s identity. Exceptions may be provided on a case-by-case basis
should the request for PA document that compliance with this requirement would
jeopardize the health, safety, or well-being of the member; AND
(4) Member has had 12 continuous months of clinician-supervised hormone therapy
appropriate to the member’s gender goals, unless hormone therapy is medically
contraindicated; OR
d. Facial Feminization or Facial Masculinization Surgical Procedures:
ONE (1) or more of the procedures listed in items (1) through (12) will be performed:
Gender Affirmation Services
6 of 29
(1) Blepharoplasty (eyelid surgery) ONLY in conjunction with other medically
necessary facial feminization or facial masculinization procedures;
(2) Brow reconstruction/brow lift;
(3) Cheek augmentation;
(4) Forehead contouring (including forehead reshaping or forehead reduction);
(5) Genioplasty (chin augmentation, chin reconstruction, or chin
reduction/narrowing);
(6) Scalp/hairline advancement;
(7) Lateral canthopexy;
(8) Surgical lip lift;
(9) Lysis intranasal synechiae;
(10) Mandibuloplasty;
(11) Osteoplasty;
(12) Rhinoplasty and septoplasty;
(13) Rhytidectomy (facelift surgery) of the forehead, cheek, and/or neck
(platysmaplasty);
(14) Suction-assisted lipectomy in conjunction with medically necessary facial
procedures; AND/OR
(15) Tracheoplasty/tracheal shave; OR
e. Hair Removal with Laser or Electrolysis:
Electrolysis and/or laser treatments for face and neck hair removal is performed by a
licensed and qualified treating clinician and ALL criteria are met in items (1) through (5):
(1) A licensed qualified health professional recommends hair removal of the face
and/or neck as part of the member’s medically necessary treatment for gender
dysphoria; AND
Gender Affirmation Services
7 of 29
(2) A letter from the clinician performing the hair removal is submitted to the Plan and
includes attestation of the medical necessity of hair removal and a summary of the
member’s care as it relates to gender dysphoria treatment; AND
(3) Documentation submitted to the Plan includes the area size and location(s) for
permanent hair removal, the type of hair removal treatment (laser or electrolysis),
and the expected timeframe and number of treatments requested. The Plan will
authorize medically necessary requests for electrolysis and/or laser ablation
treatments for medically necessary permanent hair removal of the face and/or neck for
up to 12 calendar months from the date of the authorization request. Additional
treatments require a separate Plan authorization; AND
(4) Clinician performing the hair removal has discussed risks and complications of the
proposed procedure, including the clinician’s own complication rates, and has
obtained informed consent from the member; AND
(5) Member has had 12 continuous months of clinician-supervised hormone therapy
appropriate to the member’s gender goals unless hormone therapy is medically;
OR
f. Hair removal for standard pre-operative preparation for genital gender affirmation
surgery:
Electrolysis and/or laser treatments for hair removal is performed by a licensed and
qualified treating provider and ALL criteria are met in items (1) through (4):
(1) Permanent hair removal is required as part of the standard pre-operative
preparation for genital affirming surgery(ies) and is recommended by the treating
surgeon, with documentation verifying that hair removal is medically necessary;
AND
(2) A letter from the clinician performing the hair removal is submitted to the Plan and
includes attestation of the medical necessity of hair removal and a summary of the
member’s care as it relates to gender dysphoria treatment; AND
(3) Documentation submitted to the Plan includes the area size and location(s) for
permanent hair removal, the type of hair removal treatment (laser or electrolysis),
expected timeframe and number of treatments requested, and the estimated date
of the genital gender affirmation surgical procedure(s). The Plan will authorize
medically necessary requests for electrolysis and/or laser ablation treatments for
medically necessary pre-operative permanent hair removal as standard preparation for
genital gender affirmation surgery for up to 18 calendar months from the date of the
authorization request. Additional treatments require a separate Plan authorization; AND
Gender Affirmation Services
8 of 29
(4) Clinician performing the hair removal has discussed risks and complications of the
proposed procedure, including the clinician’s own complication rates, and has
obtained informed consent from the member; OR
g. Gender Affirmation Procedures NOT Requiring Medically Necessary Permanent Hair
Removal of Graft Site:
The Plan will authorize medically necessary requests for gender affirmation surgery(ies)
up to 12 calendar months from the date of the authorization request; OR
h. Genital Gender Affirmation Procedures Requiring Medically Necessary Permanent Hair
Removal of Graft Site:
The Plan will authorize medically necessary requests for genital gender affirmation
procedure(s) that require pre-operative permanent hair removal as standard
preparation for surgery up to 18 calendar months from the date of the authorization
request.
II. The following requests require Plan Medical Director review:
A. Permanent hair removal in preparation for planned genital gender affirmation procedure if the
procedure has not yet been authorized by the Plan.
B. Hair removal when documentation from the member’s surgeon and/or qualified licensed health
provider(s) is within 13-18 calendar months of the prior authorization request and permanent
hair removal is NOT a medically necessary component of pre-operative preparation for genital
gender affirmation procedure(s). Additional documentation must be submitted to the Plan to
report the extenuating circumstances that necessitate an extension of the standard 12 calendar
month time limit.
C. Gender affirmation surgery for a member who does NOT meet DSM-5 definitive diagnosis of
persistent gender dysphoria (e.g., non-binary members who do not meet traditional diagnostic
criteria for gender dysphoria).
D. Gender affirmation services for a member unable to live in the chosen gender role full-time.
This includes members who identify as genders other than male or female. Treating provider
must submit documentation indicating why it would be clinically inappropriate to require the
member to meet this criterion and why this requirement should be waived.
E. Gender affirmation surgery and/or permanent hair removal for a member age 17 or younger on
the date of service. The Plan Medical Director will review the current version of WPATH
Standards of Care and member’s clinical situation, including but not limited to the amount of
time the adolescent member has been living in the gender congruent role, treatment timeframe
with hormone therapy, age of the member, and the requested intervention. Adolescent

Gender Affirmation Services
9 of 29
members may be eligible for interventions when adolescents and their parents (or guardian)
make informed decisions about treatment, and the service is a covered benefit for the Plan
member. Informed consent by a parent or guardian for treatment of an adolescent member
may not apply if the adolescent member is emancipated at the time the service is rendered (as
determined by state requirements).
F. Surgical revision of a previously performed gender affirmation surgery.
G. Laparoscopic prostatectomy as a component of gender affirmation surgical procedure(s).
H. Post-operative lodging is NOT routinely covered by the Plan; Plan Medical Director review is
required.
Limitations and Exclusions
A. External review will be available to the members enrolled in Qualified Health Plans,
ConnectorCare, or Employer Choice Direct products when the Plan determines that coverage
for treatment of gender dysphoria is NOT medically necessary or the Plan considers the
treatment experimental or investigational. The external review for Qualified Health Plans,
ConnectorCare, or Employer Choice Direct products will be based upon the Massachusetts
definition of medical necessity. (Source: The Commonwealth of Massachusetts, Health Policy
Commission, Memo: External Review for Denials of Coverage for Medical and/or Surgical
Treatment of Gender Dysphoria, July 2, 2015.)
B. Hair removal is ONLY covered when criteria are met in the Clinical Criteria section for the
method of hair removal (i.e., electrolysis and/or laser hair removal). Any other method of hair
removal or indication for treatment is NOT covered.
C. The Plan considers any services or surgical procedures used to reverse gender affirmation
surgery to NOT be medically necessary.
D. The following procedures/services in items 1 through 17 are NOT covered for the treatment of
gender dysphoria:
1. Blepharoplasty (eyelid surgery) NOT in conjunction with other facial feminization or facial
masculinization procedures used for the treatment of gender dysphoria; OR
2. Body contouring procedures, including abdominoplasty, liposuction, lipofilling, and/or
suction-assisted lipectomy UNLESS the treatment is listed as medically necessary in the
Clinical Criteria section (e.g., facial procedures for the treatment of gender dysphoria) and
ALL applicable clinical review criteria are met for the gender affirmation surgical procedure;
OR
3. Calf augmentation (calf implants); OR

Gender Affirmation Services
10 of 29
4. Collagen injections; OR
5. Facial feminization surgery, facial masculinization surgery, facial bone reduction, or facial
implants or injections UNLESS the treatment is specified as medically necessary in the
Clinical Criteria section and applicable clinical review criteria are met for the facial
feminizing or facial masculinizing gender affirmation surgical procedure; OR
6. Gluteal augmentation (gluteal implants and/or lipofilling); OR
7. Hair transplantation or hair reconstruction (see the Clinical Criteria section for guidelines for
hairline advancement surgery); OR
8. Laryngoplasty (technique to alter the voice tract and adjust vocal range); OR
9. Lip reduction or lip enhancement (see the Clinical Criteria section for guidelines related to
lip lift); OR
10. Osteoplasty UNLESS clinical review criteria are met for the facial feminization or facial
masculinization gender affirmation surgical procedure in the Clinical Criteria section); OR
11. Otoplasty (surgical reshaping of the outer ear); OR
12. Pectoral augmentation (pectoral implants); OR
13. Removal of redundant skin including but NOT limited to panniculectomy and/or
abdominoplasty when used for the treatment of gender dysphoria UNLESS the procedure
is listed as medically necessary in the Clinical Criteria section and applicable criteria are met;
OR
Note: Review the Plan’s medical necessity guidelines included in the Panniculectomy and
Related Redundant Skin Surgery medical policy, policy number OCA 3.722.
14. Silicone injections of the breast; OR
15. Skin resurfacing treatments including but NOT limited to chemical peels and/or
dermabrasion; OR
16. Tattooing; OR
17. Vocal cord surgery (laryngoplasty, cricothyroid approximation or shortening of the vocal
cords).
Gender Affirmation Services
11 of 29
E. Reimbursement for travel expenses is NOT covered by the Plan unless the Plan’s product-
specific criteria are met, as specified in the Non-Emergency Transportation Services medical
policy applicable for the member’s product, policy number OCA 3.191.
Variations
The Plan uses guidance from the Centers for Medicare & Medicaid Services (CMS) for medical
necessity and coverage determinations for the Plan’s Senior Care Options (SCO) members and New
Hampshire Medicare Advantage HMO members, including but not limited to national coverage
determinations (NCDs), local coverage determinations (LCDs), local coverage articles (LCAs), and
documentation included in Medicare manuals. At the time of the Plan’s most recent policy review,
NCD 140.9 states CMS has determined that no NCD is appropriate at this time for gender affirmation
surgery for Medicare beneficiaries with gender dysphoria. LCA A53793 includes billing, coding, and
treatment guidelines for gender affirmation services for gender dysphoria. Verify CMS guidelines in
effect on the date of the prior authorization request. When there is no guidance from CMS for the
requested service, Plan-adopted clinical review criteria will be used to determine the medical necessity
of the service.
Applicable Coding
The Plan utilizes up-to-date, industry-standard Current Procedural Terminology (CPT) codes, Health
Care Common Procedure Coding System (HCPCS) codes, and International Statistical Classification
of Diseases and Related Health Problems, 10th revision (ICD-10) diagnosis codes in the Plan’s medical
policies. Since these codes may be updated at different intervals than the medical policy review cycle,
the list of applicable codes included in a policy is informational only and may not be all
inclusive. Applicable codes are subject to change without prior notification and do not guarantee
member coverage or provider reimbursement. Review the Plan’s reimbursement policies for Plan
billing guidelines. Providers are responsible for obtaining prior authorization for the services specified
in the Clinical Criteria section and Limitations and Exclusions section of a medical policy, even if an
applicable code appropriately describing the service is not included in the policy’s Applicable Coding
section. Providers are expected to report all services using the most up-to-date, industry-standard
procedures and diagnosis codes at the time of the service.
ICD-10 Codes
Description: The following primary diagnosis codes apply to gender dysphoria
and require prior authorization when billed with a medically necessary procedure
code covered by the Plan for gender affirmation surgeries and/or hair removal.
Each gender affirmation surgery requires Plan prior authorization for ALL diagnosis and
procedure codes, even if coding is not included in this Applicable Coding section. See the
member’s applicable benefit document to determine coverage of services. Plan Medical
Director review is required for each gender affirmation surgery when the member has a
diagnosis of gender incongruence (without a diagnosis of gender dysphoria) for individual
consideration.
F64.0-F64.9
Gender identity disorders
Z87.890
History of sex reassignment surgery
Gender Affirmation Services
12 of 29
CPT Codes
Description: Services considered medically necessary for the treatment of
gender dysphoria if Plan clinical review criteria are met (when billed with a
primary ICD-10 diagnosis code listed above). Prior authorization is required.
11960
Insertion of tissue expander(s) for other than breast, including subsequent expansion
11970
Replacement of tissue expander with permanent prosthesis
11971
Removal of tissue expander(s) without insertion of prosthesis
14040
Adjacent tissue transfer or rearrangement, forehead, cheeks, chin, mouth, neck, axillae,
genitalia, hands and/or feet; defect 10 sq cm or less
14041
Adjacent tissue transfer or rearrangement, forehead, cheeks, chin, mouth, neck, axillae,
genitalia, hands and/or feet; defect 10.1 sq cm to 30.0 sq cm
15769
Grafting of autologous soft tissue, other, harvested by direct excision (e.g., fat, dermis,
fascia)
15771
Grafting of autologous fat harvested by liposuction technique to trunk, breasts, scalp,
arms and/or legs; 50 cc or less injectate
15772
Grafting of autologous fat harvested by liposuction technique to trunk, breasts, scalp,
arms and/or legs; each additional 50 cc injectate, or part thereof (List separately in
addition to code for primary procedure)
15820
Blepharoplasty, lower eyelid
15821
Blepharoplasty, lower eyelid; with extensive herniated fat pad
15822
Blepharoplasty, upper eyelid
15823
Blepharoplasty, upper eyelid; with excessive skin weighting down lid
15824
Rhytidectomy; forehead
Plan note: Code is NOT payable for the MassHealth and QHP products.
15825
Rhytidectomy; neck with platysmal tightening (platysmal flap, P-flap)
Plan note: Code is NOT payable for the MassHealth and QHP products.
15826
Rhytidectomy; glabellar frown lines
Plan note: Code is NOT payable for MassHealth and QHP products.
15828
Rhytidectomy; cheek, chin, and neck
Plan note: Code is NOT payable for MassHealth and QHP products.
15876
Suction assisted lipectomy; head and neck
19301
Mastectomy partial (e.g., lumpectomy, tylectomy, quadrantectomy, segmentectomy)
19303
Mastectomy, simple, complete
19318
Breast reduction
19325
Breast augmentation with implant
Plan note: Breast reconstruction for male-to-female members with persistent, well-
documented gender dysphoria may include the medically necessary surgical removal of
breast implants and/or the replacement of breast implants after implant explantation
(including when the implant was initially inserted as a component of a gender affirmation
surgery); review the criteria in the Breast Reconstruction medical policy, policy number
OCA 3.43, rather than the criteria included in this policy for Plan prior authorization
guidelines for these surgical procedures.
19350
Nipple/areola reconstruction
21120
Genioplasty; augmentation (autograft, allograft, prosthetic material)
Gender Affirmation Services
13 of 29
21121
Genioplasty; sliding osteotomy, single piece
21122
Genioplasty; sliding osteotomies, 2 or more osteotomies (e.g., wedge excision or bone
wedge reversal for asymmetrical chin)
21123
Genioplasty; sliding, augmentation with interpositional bone grafts (includes obtaining
autografts)
21125
Augmentation, mandibular body or angle; prosthetic material
21127
Augmentation, mandibular body or angle; with bone graft, onlay or interpositional
(includes obtaining autograft)
21137
Reduction forehead; contouring only
21138
Reduction forehead; contouring and application of prosthetic material or bone graft
(includes obtaining autograft)
21139
Reduction forehead; contouring and setback of anterior frontal sinus wall
21141
Reconstruction midface, LeFort I; single piece, segment movement in any direction (e.g.,
for Long Face Syndrome), without bone graft
21142
Reconstruction midface, LeFort I; 2 pieces, segment movement in any direction, without
bone graft
21143
Reconstruction midface, LeFort I; 3 or more pieces, segment movement in any direction,
without bone graft
21145
Reconstruction midface, LeFort I; single piece, segment movement in any direction,
requiring bone grafts (includes obtaining autografts)
21146
Reconstruction midface, LeFort I; 2 pieces, segment movement in any direction, requiring
bone grafts (includes obtaining autografts) (e.g., ungrafted unilateral alveolar cleft)
21147
Reconstruction midface, LeFort I; 3 or more pieces, segment movement in any direction,
requiring bone grafts (includes obtaining autografts) (e.g., ungrafted bilateral alveolar
cleft or multiple osteotomies)
21150
Reconstruction midface, LeFort II; anterior intrusion (e.g., Treacher-Collins Syndrome)
21151
Reconstruction midface, LeFort II; any direction, requiring bone grafts (includes obtaining
autografts)
21154
Reconstruction midface, LeFort III (extracranial), any type, requiring bone grafts (includes
obtaining autografts); without LeFort I
21155
Reconstruction midface, LeFort III (extracranial), any type, requiring bone grafts (includes
obtaining autografts); with LeFort I
21159
Reconstruction midface, LeFort III (extra and intracranial) with forehead advancement
(e.g., mono bloc), requiring bone grafts (includes obtaining autografts); without LeFort I
21160
Reconstruction midface, LeFort III (extra and intracranial) with forehead advancement
(e.g., mono bloc), requiring bone grafts (includes obtaining autografts); with LeFort I
21172
Reconstruction superior-lateral orbital rim and lower forehead, advancement or alteration,
with or without grafts (includes obtaining autografts)
21175
Reconstruction, bifrontal, superior-lateral orbital rims and lower forehead, advancement or
alteration (e.g., plagiocephaly, trigonocephaly, brachycephaly), with or without grafts
(includes obtaining autografts)
21179
Reconstruction, entire or majority of forehead and/or supraorbital rims; with grafts
(allograft or prosthetic material)
21180
Reconstruction, entire or majority of forehead and/or supraorbital rims; with autograft
(includes obtaining grafts)
21188
Reconstruction midface, osteotomies (other than LeFort type) and bone grafts (includes
obtaining autografts)
Gender Affirmation Services
14 of 29
21196
Reconstruction of mandibular rami and/or body, sagittal split; with internal rigid fixation
21208
Osteoplasty, facial bones; augmentation (autograft, allograft, or prosthetic implant)
21209
Osteoplasty, facial bones; reduction
21210
Graft, bone; nasal, maxillary or malar areas (includes obtaining graft)
21230
Graft; rib cartilage, autogenous, to face, chin, nose or ear (includes obtaining graft
21244
Reconstruction of mandible, extraoral, with transosteal bone plate (e.g., mandibular staple
bone plate)
21245
Reconstruction of mandible or maxilla, subperiosteal implant; partial
21246
Reconstruction of mandible or maxilla, subperiosteal implant; complete
21248
Reconstruction of mandible or maxilla, endosteal implant (e.g., blade, cylinder); partial
21249
Reconstruction of mandible or maxilla, endosteal implant (e.g., blade, cylinder); complete
21270
Malar augmentation, prosthetic material
21282
Lateral canthopexy
30400
Rhinoplasty, primary; lateral and alar cartilages and/or elevation of nasal tip
30410
Rhinoplasty, primary; complete, external parts including bony pyramid, lateral and alar
cartilages, and/or elevation of nasal tip
30420
Rhinoplasty, primary; including major septal repair
30430
Rhinoplasty, secondary; minor revision (small amount of nasal tip work)
30435
Rhinoplasty, secondary; intermediate revision (bony work with osteotomies)
30450
Rhinoplasty, secondary; major revision (nasal tip work and osteotomies )
30460
Rhinoplasty for nasal deformity secondary to congenital cleft lip and/or palate, including
columellar lengthening; tip only
30462
Rhinoplasty for nasal deformity secondary to congenital cleft lip and/or palate, including
columellar lengthening; tip, septum and osteotomies
30465
Repair of nasal vestibular stenosis (e.g., spreader grafting, lateral nasal wall
reconstruction)
30520
Septoplasty or submucous resection, with or without cartilage scoring, contouring or
replacement with graft
30560
Lysis intranasal synechia
31599
Unlisted procedure, trachea, bronchi
31750
Tracheoplasty; cervical
Plan note: Code used for trachea shaving for male-to-female transition.
40799
Unlisted procedure, lips
Plan note: Code used for lip lift.
49329
Peritoneal Flap, Unlisted
53410
Urethroplasty, 1-stage reconstruction of male anterior urethra
53415
Urethroplasty, transpubic or perineal, 1-stage, for reconstruction or repair of prostatic or
membranous urethra
53420
Urethroplasty, 2-stage reconstruction or repair of prostatic or membranous urethra; first
stage
53425
Urethroplasty, 2-stage reconstruction or repair of prostatic or membranous urethra;
second stage
53430
Urethroplasty, reconstruction of female urethra
53450
Urethromeatoplasty, with mucosal advancement
54120
Amputation of penis; partial
Gender Affirmation Services
15 of 29
54125
Amputation of penis; complete
54400
Insertion of penile prosthesis; non-inflatable (semi-rigid)
54401
Insertion of penile prosthesis; inflatable (self-contained)
54405
Insertion of multi-component inflatable penile prosthesis, including placement of pump,
cylinders, and reservoir
54520
Orchiectomy, simple (including subcapsular), with or without testicular prosthesis, scrotal
or inguinal approach
54660
Insertion of testicular prosthesis (separate procedure)
54690
Laparoscopy, surgical; orchiectomy
55175
Scrotoplasty; simple
55180
Scrotoplasty; complicated
55970
Intersex surgery; male to female
Plan note: Series of staged procedures to remove penis and create vagina.
55980
Intersex surgery; female to male
Plan note: Series of staged procedures to remove or close vagina and for penis and
testicles.
56620
Vulvectomy simple; partial
56625
Vulvectomy simple; complete
56800
Plastic repair of introitus
56805
Clitoroplasty for intersex state
56810
Perineoplasty, repair of perineum, non-obstetrical (separate procedure)
57106
Vaginectomy, partial removal of vaginal wall
57107
Vaginectomy, partial removal of vaginal wall; with removal of paravaginal tissue (radical
vaginectomy)
57110
Vaginectomy, complete removal of vaginal wall
57111
Vaginectomy, complete removal of vaginal wall; with removal of paravaginal tissue (radical
vaginectomy)
57291
Construction of artificial vagina; without graft
57292
Construction of artificial vagina; with graft
57335
Vaginoplasty for intersex state
58150
Total abdominal hysterectomy (corpus and cervix), with or without removal of tube(s),
with or without removal of ovary(s)
58180
Supracervical abdominal hysterectomy (subtotal hysterectomy) with or without removal
of tube(s), with or without removal of ovary(s)
58260
Vaginal hysterectomy, for uterus 250g or less
58262
Vaginal hysterectomy, for uterus 250g or less; with removal of tube(s), and/or ovary(s)
58275
Vaginal hysterectomy, with total or partial vaginectomy
58290
Vaginal hysterectomy, for uterus greater than 250g
58291
Vaginal hysterectomy, for uterus greater than 250g; with removal of tube(s) and/or
ovary(s)
58541
Laparoscopy, surgical, supracervical hysterectomy, for uterus 250g or less
58542
Laparoscopy, surgical, supracervical hysterectomy, for uterus 250g or less; with removal of
tube(s) and/or ovary(s)
58543
Laparoscopy, surgical, supracervical hysterectomy, for uterus greater than 250g
Gender Affirmation Services
16 of 29
58544
Laparoscopy, surgical, supracervical hysterectomy, for uterus greater than 250g; with
removal of tube(s) and/or ovary(s)
58550
Laparoscopy, surgical, with vaginal hysterectomy, for uterus 250g or less
58552
Laparoscopy, surgical, with vaginal hysterectomy, for uterus 250 grams or less; with
removal of tube(s) and/or ovary(s)
58553
Laparoscopy, surgical with vaginal hysterectomy, for uterus greater than 250g
58554
Laparoscopy, surgical, with vaginal hysterectomy, for uterus greater than 250 grams; with
removal of tube(s) and/or ovary(s)
58570
Laparoscopy, surgical, with total hysterectomy, for uterus 250g or less
58571
Laparoscopy, surgical, with total hysterectomy, for uterus 250 g or less; with removal of
tube(s) and/or ovary(s)
58572
Laparoscopy, surgical, with total hysterectomy, for uterus greater than 250g
58573
Laparoscopy, surgical, with total hysterectomy, for uterus greater than 250 g; with
removal of tube(s) and/or ovary(s)
58661
Laparoscopy, surgical; with lysis of adhesions (salpingolysis, ovariolysis) (separate
procedure); with removal of adnexal structures (partial or total oophorectomy and/or
salpingectomy)
58720
Salpingo-oophorectomy, complete or partial, unilateral or bilateral (separate procedure)
58940
Oophorectomy, partial or total, unilateral or bilateral
67900
Repair of brow ptosis (supraciliary, mid-forehead or coronal approach)
HCPCS Code
Description: Service is considered medically necessary for the treatment of
gender dysphoria if Plan criteria are met and is billed with a primary ICD-10
diagnosis code listed above. Prior authorization is required.
L8600
Implantable breast prosthesis, silicone or equal
CPT Codes
Description: The following services require Plan Medical Director review and
approval when used for the treatment of gender dysphoria (and billed with a
primary ICD-10 diagnosis code listed above). Prior authorization is required.
19316
Mastopexy
19380
Revision of reconstructed breast (e.g., significant removal of tissue, re-advancement
and/or re-inset of flaps in autologous reconstruction or significant capsular revision
combined with soft tissue excision in implant-based reconstruction)
31587
Laryngoplasty, cricoid split, without graft placement
55866
Laparoscopy, surgical prostatectomy, retropubic radical, including nerve sparing, includes
robotic assistance, when performed
57295
Revision (including removal) of prosthetic vaginal graft; vaginal approach
57296
Revision (including removal) of prosthetic vaginal graft; open abdominal approach
57426
Revision (including removal) of prosthetic vaginal graft, laparoscopic approach
CPT Codes
Description: Coverage guidelines based on the indication for treatment and type
of service provided (when billed with a primary ICD-10 diagnosis code listed
above for gender dysphoria). Prior authorization is required.
17380
Electrolysis epilation, each 30 minutes
17999
Unlisted procedure, skin, mucous membrane and subcutaneous tissue
Gender Affirmation Services
17 of 29
Plan note: Code used when billing for laser ablation for hair removal on a skin graft donor
site for a genital gender affirmation surgery.
CPT Codes
Description: Services NOT considered medically necessary for the treatment of
gender dysphoria (and billed with a primary ICD-10 diagnosis code listed above).
Prior authorization is required.
11950
Subcutaneous injection of filling material (e.g., collagen); 1 cc or less
11951
Subcutaneous injection of filling material (e.g., collagen); 1.1 to 5.0 cc
11952
Subcutaneous injection of filling material (e.g., collagen); 5.1 to 10 cc or less
11954
Subcutaneous injection of filling material (e.g., collagen); over 10 cc
15775
Punch graft for hair transplant; 1-15 punch grafts
15776
Punch graft for hair transplant; more than 15 punch grafts
15780
Dermabrasion; total face (e.g., for acne scarring, fine wrinkling, rhytids, general keratosis)
15781
Dermabrasion; segmental, face
15782
Dermabrasion; regional, other than face
15783
Dermabrasion; superficial, any site (e.g., tattoo removal)
15786
Abrasion; single lesion (e.g., keratosis, scar)
15787
Abrasion; each additional 4 lesions or less (List separately in addition to code for primary
procedure)
15788
Chemical peel, facial; epidermal
15789
Chemical peel, facial; dermal
15792
Chemical peel, nonfacial; epidermal
15793
Chemical peel, nonfacial; dermal
15830
Excision, excessive skin and subcutaneous tissue (including lipectomy); abdomen,
infraumbilical panniculectomy
15832
Excision, excessive skin and subcutaneous tissue (including lipectomy); thigh
15833
Excision, excessive skin and subcutaneous tissue (including lipectomy); leg
15834
Excision, excessive skin and subcutaneous tissue (including lipectomy); hip
15835
Excision, excessive skin and subcutaneous tissue (including lipectomy); buttock
15836
Excision, excessive skin and subcutaneous tissue (including lipectomy); arm
15837
Excision, excessive skin and subcutaneous tissue (including lipectomy); forearm or hand
15838
Excision, excessive skin and subcutaneous tissue (including lipectomy); submental fat pad
15839
Excision, excessive skin and subcutaneous tissue (including lipectomy); other area
15847
Excision, excessive skin and subcutaneous tissue (includes lipectomy), abdomen (e.g.,
abdominoplasty) (includes umbilical transposition and fascial plication)
15877
Suction assisted lipectomy; trunk
15878
Suction assisted lipectomy; upper extremity
15879
Suction assisted lipectomy; lower extremity
References
American Academy of Child & Adolescent Psychiatry (AACAP). Adelson SL; AACAP Committee on
Quality Issues (CQI): Walter HJ, Bukstein OG, Bellonci C, Beson RS, Chisman A, Farchione TR,
Hamilton J, Keable H, Kinlan J, Quiterio N, Schoettle U, Siegel M, Stock S; Medicus J. Practice
Parameter on Gay, Lesbian, or Bisexual Sexual Orientation, Gender Nonconformity, and Gender
Discordance in Children and Adolescents. J Am Acad Child Adolesc Psychiatry. 2012 Sep;51(9):957-74.
doi: 10.1016/j.jaac.2012.07.004. PMID: 22917211.

Gender Affirmation Services
18 of 29
American Academy of Child & Adolescent Psychiatry (AACAP). AACAP Sexual Orientation and Gender
Identity Issues Committee. Conversion Therapy Policy (Lack of Evidence). 2018 Feb.
American Academy of Pediatrics (AAP). Levine DA, the Committee on Adolescence. Office-Based
Care for Lesbian, Gay, Bisexual, Transgender, and Questioning Youth. Pediatrics. 2013 Jul;132(1):e297-
313. doi:10.1542/peds.2013-1283. PMID: 23796737.
American Academy of Pediatrics (AAP). Rafferty J; Committee on Psychosocial Aspects of Child and
Family Health; Committee on Adolescence; Section on Lesbian, Gay, Bisexual, and Transgender Health
and Wellness. Ensuring Comprehensive Care and Support for Transgender and Gender-Diverse
Children and Adolescents. Pediatrics. 2018 Oct;142(4). pii: e20182162. doi: 10.1542/peds.2018-2162.
Epub 2018 Sep 17. PMID: 30224363.
American College of Obstetricians and Gynecologists (ACOG). Committee Opinion Number 512.
Healthcare for Transgender Individuals. 2011 Dec. Obstet Gynecol. 2011 Dec;118(6):1454-1458. doi:
10.1097/AOG.0b013e31823ed1c1. PMID: 22105293.
American College of Obstetricians and Gynecologists (ACOG). Committee Opinion Number 685. Care
for Transgender Adolescents. Obstet Gynecol. 2017 Jan;129(1):e11-16. doi: 10.1097/
AOG.0000000000001861. PMID: 28002311.
American College of Pediatricians (ACPeds). Position Statement. Gender Dysphoria in Children. 2018
Nov.
American Medical Association (AMA). Policies on Lesbian, Gay, Bisexual, Transgender & Queer
(LGBTQ) issues.
American Psychiatric Association (APA). Byne W, Bradley S, Coleman E, Eyler AE, Green R, Menvielle
EJ, Meyer-Bahlburg HFL, Pleak RR, Tompkins DA; APA Task Force on Treatment of Gender Identity
Disorder. Report of the APA Task Force on Treatment of Gender Identity Disorder. Arch Sex
Behav. 2012 Aug;41(4):759-96. doi: 10.1007/s10508-012-9975-x. PMID: 22736225.
American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders, Fifth
Edition. APA. Arlington, VA. 2013:451-9.
American Psychiatric Association (APA). Parekh R. Help with Gender Dysphoria. 2016 Feb.
American Psychiatric Association (APA). Parekh R. What is Gender Dysphoria? 2016 Feb.
American Psychological Association (APA). APA Task Force on Guidelines for Psychological Practice
with Transgender and Gender Nonconforming People; Dickey LM, Singh AA, Bockting WO, Chang S,
Ducheny K, Edwards-Leeper L, Ehrbar RD, Fuhrmann MF, Hendricks ML, Magalhaes E. Guidelines for

Gender Affirmation Services
19 of 29
Psychological Practice with Transgender and Gender Nonconfirming People. American Psychologist.
2015 Dec;70(9):832-64. doi: 10.1037/a0039906. PMID: 26653312.
American Psychological Association (APA). APA Task Force; Schneider MS, Bockting WO, Ehrbar RD,
Lawrence AA, Rachlin K, Zucker KJ. Report of the APA Task Force on Gender Identity and Gender
Variance. 2009.
American Psychological Association (APA). Bockting W. The Psychology of Transgender. 2015 Nov 19.
American Psychological Association (APA). Transgender, Gender Identity, & Gender Expression Non-
Discrimination Resolution. 2008 Aug.
American Psychological Association (APA). Transgender People, Gender Identity and Gender
Expression. What does transgender mean? 2014.
Beek TF, Cohen-Kettenis PT, Bouman WP, de Vries ALC, Steensma TD, Witcomb GL, Arcelus J,
Richards C, De Cuypere G, Kreukels BP. Gender Incongruence of Childhood: Clinical Utility and
Stakeholder Agreement with the World Health Organization’s Proposed ICD-11 Criteria. PLoS One.
2017 Jan 12;12(1):e0168522. doi: 10.1371/journal.pone.0168522. eCollection 2017. PMID: 28081569.
Beek TF, Cohen-Kettenis PT, Kreukels BP. Gender incongruence/gender dysphoria and its
classification history. Int Rev Psychiatry. 2016;28(1):5-12. doi: 10.3109/09540261.2015.1091293. Epub
2015 Nov 19. PMID: 26782319.
Bekeny JC, Zolper EG, Fan KL, Del Corral G. Breast augmentation for transfeminine patients: methods,
complications, and outcomes. Gland Surg. 2020 Jun;9(3):788-796. doi: 10.21037/gs.2020.03.18.
PMID: 32775269.
Bradford NJ, Rider GN, Spencer KG. Hair removal and psychological well-being in transfeminine adults:
associations with gender dysphoria and gender euphoria. J Dermatolog Treat. 2021 Sep;32(6):635-42.
doi: 10.1080/09546634.2019.1687823. Epub 2019 Nov 22. PMID: 31668100.
Bradley SJ, Zucker KJ. Gender identity disorder: a review of the past 10 years. J Am Acad Child
Adolesc Psychiatry. J Am Acad Child Adolesc Psychiatry. 1997 Jul;36(7):872-80. doi:
10.1097/00004583-199707000-00008. PMID: 9204664.
Centers for Disease Control and Prevention (CDC). Lesbian, Gay, Bisexual, and Transgender Health.
Resources.
Center of Excellence for Transgender Health. Deutsch MB. Guidelines for the Primary and Gender-
Affirming Care of Transgender and Gender Nonbinary People. 2016 Jun 17.

Gender Affirmation Services
20 of 29
Centers for Medicare & Medicaid Services (CMS). Local Coverage Article (LCA) A53793. Billing and
Coding: Gender Reassignment Services for Gender Dysphoria. 2015 Oct 1. Revision Effective Date 2021
Jan 1.
Centers for Medicare & Medicaid Services (CMS). Manuals. Publication # 100-02. Medicare Benefit
Policy Manual.
Centers for Medicare & Medicaid Services (CMS). Manuals. Publication # 100-03. Medicare National
Coverage Determinations (NCD) Manual.
Centers for Medicare & Medicaid Services (CMS). Medicare Coverage Database (MCD).
Centers for Medicare & Medicaid Services (CMS). National Coverage Determination (NCD) 140.9.
Gender Dysphoria and Gender Reassignment Surgery. 2017 Apr 4.
Chung KC. Operative Techniques in Plastic Surgery. First Edition. 2018. Lippincott Williams & Wilkins.
ISBN: 978-1-49-633950-8.
Commonwealth of Massachusetts. Executive Office of Health and Human Services (EOHHS).
MassHealth Guidelines for Medical Necessity Determination for Gender Affirming Surgery. MNG-
GAS-0921. 2021 Sep 1.
Commonwealth of Massachusetts. Executive Office of Health and Human Services (EOHHS).
MassHealth Guidelines for Medical Necessity Determination for Hair Removal. MNG-HR-0921. 2021
Sep 1.
Commonwealth of Massachusetts. Executive Office of Health and Human Services (EOHHS).
MassHealth Provider Bulletins.
Commonwealth of Massachusetts. Executive Office of Health and Human Services (EOHHS).
MassHealth Provider Manuals.
Commonwealth of Massachusetts. Executive Office of Health and Human Services (EOHHS).
MassHealth Transmittal Letters.
Commonwealth of Massachusetts. Massachusetts Law about Emancipation of Minors.
Dittrich R, Binder H, Cupisti S, Hoffmann I, Beckmann MW, Mueller A. Endocrine Treatment of Male-to-
Female Transsexuals Using Gonadotropin-Releasing Hormone Agonist. Exp Clin Endocrinol
Diabetes. 2005 Dec;113(10):586-92. doi: 10.1055/s-2005-865900. PMID: 16320157.
Dubov A, Fraenkel L. Facial Feminization Surgery: The Ethics of Gatekeeping in Transgender Health.
Amer J Bioethics. 2018 Dec:18(12):3-9. doi: 10.1080/15265161.2018.1531159.

Gender Affirmation Services
21 of 29
Endocrine Society. Corrigendum for “Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent
Persons: An Endocrine Society Clinical Practice Guideline.” J Clin Endocrinol Metab. 2018 Feb
1;103(2):699. doi.org/10.1210/jc.2017-02548. PMID: 29244095.
Endocrine Society. Hembree WC, Cohen-Kettenis PT, Gooren L, Hannema SE, Meyer WJ, Murad MH,
Rosenthal SM, Safer JD, Tangpricha V, T'Sjoen GG. Endocrine Treatment of Gender-
Dysphoric/Gender-Incongruent Persons: An Endocrine Society Clinical Practice Guideline. J Clin
Endocrinol Metab. 2017 Nov 1;102(11):3869-3903. doi: 10.1210/jc.2017-01658. Erratum in: J Clin
Endocrinol Metab. 2018 Feb 1;103(2):699. J Clin Endocrinol Metab. 2018 Jul 1;103(7):2758-59. PMID:
28945902.
Feldman J, Deutsch MB. Primary care of transgender individuals. UpToDate. Updated 2019 Oct 18.
Fernandez JD, Tannock LR. Metabolic Effects of Hormone Therapy in Transgender Patients. Endocr
Pract. 2016 Apr;22(4):383-8. doi: 10.4158/EP15950.OR. Epub 2015 Nov 17. PMID: 26574790.
Ferrando CU, Zhao LC, Nikolavsky D. Transgender surgery: Female to male. UptoDate. Updated 2022
Apr.
Hadj-Moussa M, Agarwal S, Ohl DA, Kuzon WM Jr. Masculinizing Genital Gender Confirmation Surgery.
Sex Med Rev. 2019 Jan;7(1):141-155. doi: 10.1016/j.sxmr.2018.06.004. Epub 2018 Aug 16. PMID:
30122339.
Hancock AB, Krissinger J, Owen K. Voice perceptions and quality of life of transgender people. J Voice.
2011 Sep;25(5):553-8. doi: 10.1016/j.jvoice.2010.07.013. Epub 2010 Nov 4. J Voice. 2011. PMID: 21051199.
Hayes. Health Technology Assessment. Sex Reassignment Surgery for the Treatment of Gender
Dysphoria. Dallas, TX: Hayes; 2017 Aug 1. Annual Review 2021 Jul 27.
Horbach SE, Bouman MB, Smit JM, Özer M, Buncamper ME, Mullender MG. Outcome of Vaginoplasty
in Male-to-Female Transgenders: A Systematic Review of Surgical Techniques. J Sex Med. 2015
Jun;12(6):1499-512. doi: 10.1111/jsm.12868. Epub 2015 Mar 26. PMID: 25817066.
The Joint Commission. Advancing Effective Communication, Cultural Competence, and Patient- and
Family-Centered Care for the Lesbian, Gay, Bisexual, and Transgender (LGBT) Community. A Field
Guide. 2014 Apr 3.
Kailas M, Lu HMS, Rothman EF, Safer JD. Prevalence and Types of Gender-Affirming Surgery Among
a Sample of Transgender Endocrinology Patients Prior to State Expansion of Insurance Coverage.
Endocr Pract. 2017 Jul;23(7):780-786. doi: 10.4158/EP161727.OR. Epub 2017 Apr 27. PMID: 28448757.
Lee J, Lee S. Facial Contouring Surgery-Mandibuloplasty: Genioplasty and Mandible Angle
Correction. Plast Reconstr Surg Glob Open. 2017 Oct;5(10):e1296. doi:10.1097/
GOX.0000000000001296. PMID: 29184722.
Gender Affirmation Services
22 of 29
Mañero I, Labanca T, Triviño JM. Aesthetic Refinements after Radial Free Flap Phalloplasty: Optimizing
the Donor Site and the Phallus. Plast Reconstr Surg Glob Open. 2017 Dec 28;5(12):e1611. doi:
10.1097/GOX.0000000000001611. eCollection 2017 Dec. PMID: 29632786.
Marks DH, Hagigeorges D, Manatis-Lornell AJ, Dommasch E, Senna MM. J Cosmet Dermatol. Excess
hair, hair removal methods, and barriers to care in gender minority patients: A survey study. J Cosmet
Dermatol. 2020 Jun;19(6):1494-1498. doi: 10.1111/jocd.13164. Epub 2019 Sep 25. 2020. PMID: 31553137.
Morrison SD, Capitán-Cañadas F, Sánchez-García A, Ludwig DC, Massie JP, Nolan IT, Swanson M,
Rodríguez-Conesa M, Friedrich JB, Cederna PS, Bellinga RJ, Simon D, Capitán L, Satterwhite T.
Prospective Quality-of-Life Outcomes after Facial Feminization Surgery: An International Multicenter
Study. Plastic and Reconstructive Surgery: 2020 June;145(6):1499-509. doi: 10.1097/
PRS.0000000000006837. PMID: 32459779.
National Center for Transgender Equality. Transgender Rights Toolkit: A Legal Guide for Trans People
and Their Allies (Transgender Parents), Lambda. 2015 Jan 14.
National LGBT Health Education Center. A Program of the Fenway Institute. Collecting Sexual
Orientation and Gender Identity Data.
National LGBT Health Education Center. A Program of the Fenway Institute. Sexual Orientation and
Gender Identity Questions: Information for Patients.
National LGBT Health Education Center. A Program of the Fenway Institute. Understanding the Health
Needs of LGBT People.
New Hampshire Department of Health and Human Services. Billing Manuals.
New Hampshire Department of Health and Human Services. Provider Notices.
New Hampshire Legal Aid. Legal Information, Referrals, and Pro Se Assistance. Emancipation.
Nuttbrock L, Hwahng S, Bockting W, Rosenblum A, Mason M, Macri M, Becker J. Psychiatric impact of
gender-related abuse across the life course of male-to-female transgender persons. J Sex Res. 2010
Jan;47(1):12-23. doi: 10.1080/00224490903062258. PMID: 19568976.
Olson-Kennedy J, Forcier M. Management of transgender and gender-diverse children and
adolescents. UpToDate. 2022 Apr.
Reed GM, Drescher J, Krueger RB, Atalla E, Cochran SD, First MB, Cohen-Kettenis PT, Arango-de
Montis I, Parish SJ, Cottler S, Briken P, Saxena S. Disorders related to sexuality and gender identity in
the ICD‐ 11: revising the ICD‐ 10 classification based on current scientific evidence, best clinical
practices, and human rights considerations. World Psychiatry. 2016 Oct;15(3):205-221. doi:
10.1002/wps.20354. Erratum in: World Psychiatry. 2017 Jun;16(2):220. PMID: 27717275.

Gender Affirmation Services
23 of 29
Salgado CJ, AlQattan H, Nugent A, Gerth D, Kassira W, McGee CS, Wo L. Feminizing the Face:
Combination of Frontal Bone Reduction and Reduction Rhinoplasty. Case Rep Surg. 2018 Jul
2;2018:1947807. doi: 10.1155/2018/1947807. eCollection 2018. PMID: 30057846.
Salgado CJ, Nugent AG, Satterwaite T, Carruthers KH, Joumblat NR. Gender Reassignment:
Feminization and Masculinization of the Neck. Clin Plast Surg. 2018 Oct;45(4):635-45. doi:
10.1016/j.cps.2018.06.006. Epub 2018 Aug 10. PMID: 30268248.
Schwarz K, Fontanari AMV, Schneider MA, Borba Soll BM, da Silva DC, Spritzer PM, Kazumi Yamaguti
Dorfman ME, Kuhl G, Costa AB, Cielo CA, Villas Bôas AP, Lobato MIR. Laryngeal surgical treatment in
transgender women: A systematic review and meta-analysis. Laryngoscope 2017 Nov;127(11):2596-
603. Epub 2017 Jul 3 doi: 10.1002/lary.26692. PMID: 28671273.
Seal LJ, Franklin S, Richards C, Shishkareva A, Sinclaire C, Barrett J. Predictive Markers for
Mammoplasty and a Comparison of Side Effect Profiles in Transwomen Taking Various Hormonal
Regimens. J Clin Endocrinol Metab. 2012 Dec;97(12):4422-8. doi: 10.1210/jc.2012-2030. Epub 2012 Oct
9. PMID: 23055547.
Society for Adolescent Health and Medicine (SAHM). Reitman DS, Austin B, Belkind U, Chaffee T,
Hoffman ND, Moore E, Morris R, Olson J, Ryan C. Recommendations for promoting the health and
well-being of lesbian, gay, bisexual, and transgender adolescents: a position paper of the SAHM. J
Adolesc Health. 2013 Apr;52(4):506-10. doi: 10.1016/j.jadohealth.2013.01.015. PMID: 23521897.
Soll BM, Robles-García R, Brandelli-Costa A, Mori D, Mueller A, Vaitses-Fontanari AM, Cardoso-da-
Silva D, Schwarz K, Abel-Schneider M, Saadeh A, Lobato MI. Gender incongruence: a comparative
study using ICD-10 and DSM-5 diagnostic criteria. Braz J Psychiatry. 2017 Oct 2;40(2):174-80. doi:
10.1590/1516-4446-2016-2224. Print Apr-June 2018. PMID: 28977069.
Spack NP, Edwards-Leeper L, Feldman HA, Leibowitz S, Mandel F, Diamond DA, Vance SR.
Children and adolescents with gender identity disorder referred to a pediatric medical center.
Pediatrics. 2012 Mar;129(3):418-25. doi: 10.1542/peds.201. 1-0907. Epub 2012 Feb 20. PMID: 22351896.
Tangpricha V, den Heijer M. Oestrogen and anti-androgen therapy for transgender women. Lancet
Diabetes Endocrinol. 2017 Apr;5(4):291-300. doi: 10.1016/S2213-8587(16)30319-9. Epub 2016 Dec
2. PMID: 27916515.
Tangpricha V, Safer JD. Transgender men: Evaluation and management. UpToDate. 2022 Apr.
Tangpricha V, Safer JD. Transgender women: Evaluation and management. UpToDate. 2022 Apr.
Thomas JP, Macmillan C. Feminization laryngoplasty: assessment of surgical pitch elevation. Eur Arch
Otorhinolaryngol. 2013 Sep;270(10):2695-700. doi: 10.1007/s00405-013-2511-3. Epub 2013 Apr 30.
PMID: 23632870.
Gender Affirmation Services
24 of 29
Unger CA. Hormone therapy for transgender patients. Transl Androl Urol. 2016 Dec;5(6):877–84.
doi: 10.21037/tau.2016.09.04. PMID: 28078219.
Vance SR, Ehrensaft D, Rosenthal SM. Psychological and Medical Care of Gender Nonconforming
Youth. Pediatrics. 2014 Dec;134(6):1184-92. doi: 10.1542/peds.2014-0772. Epub 2014 Nov 17. PMID:
25404716.
Wierckx K, Gooren L, T'sjoen G. Clinical Review: Breast Development in Trans Women Receiving Cross-
Sex Hormones. J Sex Med. 2014 May;11(5):1240-7. doi: 10.1111/jsm.12487. Epub 2014 Mar 12. PMID:
24618412.
The World Professional Association for Transgender Health (WPATH). Position Statement on Medical
Necessity of Treatment, Sex Reassignment, and Insurance Coverage in the U.S.A. 2016 Dec 21.
The World Professional Association for Transgender Health (WPATH). Standards of Care for the
Health of Transsexual, Transgender, and Gender-Nonconforming People. 7th Version.
Zhang WR, Garrett GL, Arron ST, Garcia MM. Laser hair removal for genital gender affirming surgery.
Transl Androl Urol. 2016 Jun;5(3):381–7. doi: 10.21037/tau.2016.03.27. PMID: 27298787.
Zucker KJ. The DSM diagnostic criteria for gender identity disorder in children. Arch Sex Behav. 2010
Apr;39(2):477-98. doi: 10.1007/s10508-009-9540-4. PMID: 19842027.
Next Review Date
04/01/23
Authorizing Entity
MPCTAC
Appendix
Appendix: Policy History
Disclaimer Information:
Plan refers to Boston Medical Center Health Plan, Inc. which operates under the trade name WellSense Health Plan. Medical
Policies are the Plan’s guidelines for determining the medical necessity of certain services or supplies for purposes of
determining coverage. These Policies may also describe when a service or supply is considered experimental or
investigational, or cosmetic. In making coverage decisions, the Plan uses these guidelines and other Plan Policies, as well as
the Member’s benefit document, and when appropriate, coordinates with the Member’s health care Providers to consider the
individual Member’s health care needs.
Plan Policies are developed in accordance with applicable state and federal laws and regulations, and accrediting organization
standards (including NCQA). Medical Policies are also developed, as appropriate, with consideration of the medical necessity
definitions in various Plan products, review of current literature, consultation with practicing Providers in the Plan’s service
area who are medical experts in the particular field, and adherence to FDA and other government agency policies. Applicable
Gender Affirmation Services
25 of 29
state or federal mandates, as well as the Member’s benefit document, take precedence over these guidelines. Policies are
reviewed and updated on an annual basis, or more frequently as needed. Treating providers are solely responsible for the
medical advice and treatment of Members.
The use of this Policy is neither a guarantee of payment nor a final prediction of how a specific claim(s) will be adjudicated.
Reimbursement is based on many factors, including member eligibility and benefits on the date of service; medical necessity;
utilization management guidelines (when applicable); coordination of benefits; adherence with applicable Plan policies and
procedures; clinical coding criteria; claim editing logic; and the applicable Plan – Provider agreement.
Gender Affirmation Services
26 of 29
Appendix: Policy History
Original Approval Date
Original Effective
Date* and Version
Number
Policy Owner
Original Policy
Approved by
Regulatory Approval: N/A
Internal Approval:
03/18/15: Medical Policy, Criteria, and
Technology Assessment Committee
(MPCTAC)
04/08/15: Quality Improvement Committee
(QIC)
07/01/15
Version 1
Medical Policy
Manager as Chair
of MPCTAC
MPCTAC and QIC
*Effective Date for QHP Commercial Product: 01/01/12
*Effective Date for NH Medicaid Product: 07/01/17
*Effective Date for Senior Care Options Product: 01/01/16
*Effective Date for NH Medicare Advantage HMO Product: 01/01/22
Policy title Gender Reassignment Surgery from 01/01/16 to 05/31/18. Policy title changed to Gender Affirmation
Surgeries from 06/01/18 to 12/31/21. Policy title changed to Gender Affirmation Services as 01/01/22.
Policy Revisions History
Review
Date
Summary of Revisions
Revision
Effective Date
and Version
Number
Approved by
09/01/15
Review for effective date 01/01/16. Updated
criteria in the Medical Policy Statement and
Limitations sections. Removed requirement for 18
months of treatment for gender dysphoria. Added
guidelines on external review for services denied
by the Plan when members are enrolled in
Qualified Health Plans, ConnectorCare, and/or
Employer Choice Direct products. Update the
Summary, Clinical Background Information,
Definitions, and References sections and the list of
applicable products.
01/01/16
Version 2
09/16/15: MPCTAC
10/14/15: QIC
11/25/15
Review for effective date 01/01/16. Updated
language in the Applicable Coding section.
01/01/16
Version 3
11/25/15: MPCTAC
(electronic vote)
12/09/15: QIC
04/01/16
Review for effective date 08/01/16. Revised the
Definitions, Clinical Background Information,
References, and Reference to Applicable Laws
and Regulations sections. Removed ICD9 codes,
added CPT code 17380 as applicable code, and
added a Plan not in the Applicable Coding section.
08/01/16
Version 4
04/20/16: MPCTAC
05/23/16: QIC
Gender Affirmation Services
27 of 29
Policy Revisions History
Revised criteria in the Medical Policy Statement
and Limitations sections.
07/05/16
Review for effective date 10/01/16. Revised
criteria in the Medical Policy Statement and
Limitations section. Revised the applicable code
list and added Plan notes to codes. Updated
Summary and References sections.
10/01/16
Version 5
07/05/16: MPCTAC
(electronic vote)
07/13/16: QIC
09/01/16
Review for effective date 10/01/16. Added
reference to the CMS Decision Memo for Gender
Dysphoria and Gender Reassignment Surgery
(CAG-00446N) effective 08/30/16 in the Clinical
Background Information and References sections.
CMS industry-wide update with no change to
criteria and/or the applicable code list for Plan
members (including members enrolled in a SCO
product).
10/01/16
Version 6
Not applicable
because industry-
wide update of CMS
guidelines with no
change to criteria
and/or the applicable
code list
09/28/16
Review for effective date 11/01/16. Administrative
changes made to clarify language related to
gender. Revised Definitions section.
11/01/16
Version 7
09/30/16: MPCTAC
(electronic vote)
10/12/16: QIC
06/01/17
Review for effective date 07/01/17. Added the NH
Medicaid product as applicable new product for
this policy as of 07/01/17 with the necessary
administrative changes made to the Medical Policy
Statement, Summary, Definitions, Clinical
Background Information, References, and
Reference to Applicable Laws and Regulations
sections. NH Medicaid criteria added in product-
specific Medical Policy Statement section and
product-specific Limitations section.
07/01/17
Version 8
06/21/17: MPCTAC
05/01/17
Review for effective date 08/01/17. Criteria for
MA products were revised in the Medical Policy
Statement section in 05/17 (with adequate
provider notification); new criteria are effective
08/01/17 for MA products. Administrative
changes made to the Summary, Definitions, and
References sections.
08/01/17
Version 9
05/17/17: MPCTAC
06/01/17
Review for effective date 08/01/17. Administrative
change made to combine criteria in the Medical
Policy Statement sections and in the Limitations
sections for all MA products and NH Medicaid
product (since all criteria are consistent among
Plan products as of 08/01/17). Administrative
change made to the Limitations section to be
consistent with the Applicable Coding section.
08/01/17
Version 10
06/21/17: MPCTAC
03/01/18
Review for effective date 06/01/18. Revised policy
title. Administrative changes made to the Policy
06/01/18
Version 11
03/21/18: MPCTAC
Gender Affirmation Services
28 of 29
Policy Revisions History
Summary, Description of Item or Service,
Definitions, Clinical Background Information,
References, and Other Applicable Policies
sections. Criteria revised in the Medical Policy
Statement and Limitations sections. Coding
updated and Plan notes revised in the Applicable
Coding section.
05/01/19
Review for effective date 08/01/19.
Administrative changes made to the Policy
Summary, Description of Item or Service, Clinical
Background Information, References, Other
Applicable Policies, and Reference to Applicable
Laws and Regulations sections. Criteria updated
in the Medical Policy Statement and Limitations
sections. Coding updated in the Applicable
Coding section.
08/01/19
Version 12
05/15/19: MPCTAC
12/01/19
Review for effective date 01/01/20. Industry-wide
update to coding (as a code deletion) included in
the Applicable Coding section.
01/01/20
Version 13
Not applicable
because industry-
wide code changes
04/01/20
Review for effective date 08/01/20.
Administrative changes made to the Definitions,
References, and Reference to Applicable Laws
and Regulations sections. Criteria revised in the
Medical Policy Statement and Limitations
sections. Coding updated in the Applicable
Coding section.
08/01/20
Version 14
04/15/20: MPCTAC
12/01/20
Review for effective date 01/01/21. Industry-wide
updates to coding in the Applicable Coding
section. Administrative changes made to the
Limitations and Other Applicable Policies sections.
01/01/21
Version 15
Not applicable
because industry-
wide code changes;
12/16/20: MPCTAC
review
01/01/21
Review for effective date 02/01/21. Revised
criteria in the Medical Policy Statement section.
02/01/21
Version 16
01/22/21: MPCTAC
(electronic vote)
04/01/21
Review for effective date 07/01/21. Revised
criteria in the Medical Policy Statement and
Limitations sections. Administrative changes
made to the Policy Summary, Description of Item
or Service, Definitions, Clinical Background
Information, and References sections. Updated
the applicable code list.
07/01/21
Version 17
04/21/21: MPCTAC
10/01/21
Review for effective date 01/01/22.
Adopted new medical policy template; removed
administrative sections, Medical Policy Statement
section renamed Clinical Criteria section, and
Limitations section renamed Limitations and
Exclusions section. Administrative changes made
01/01/22
Version 18
Version 18
replaced with
version 19 as of
10/20/21: MPCTAC
Gender Affirmation Services
29 of 29
Policy Revisions History
to the Policy Summary and References sections.
Criteria revised in the Clinical Criteria and
Limitations and Exclusions sections. Coding
revised in the Applicable Coding section.
01/01/22 and
version 18 not
implemented
11/01/21
Review for effective date 01/01/22. Administrative
changes made to the Policy Summary, Clinical
Criteria, Limitations, and Applicable Coding
sections. Criteria and coding for voice therapy
used for the treatment of gender dysphoria moved
from the Plan’s speech therapy medical policies to
this policy with Plan notification (rather than prior
authorization) required when applicable coding
guidelines followed. Revised policy title.
01/01/22
Version 19
Version 19
replaced version
18 as of 01/01/22
and all revisions
in version 18
adopted
11/30/21: MPCTAC
(electronic vote)
05/01/22
Review for effective date 08/01/22.
Administrative changes made to the Policy
Summary, Clinical Criteria, Limitations, References
and Applicable Coding sections. Added CPT codes
49329 and 53450. Non-material changes made to
Clinical Criteria and Limitations and Exclusions
sections.
08/01/22
Version 20
05/11/22: MPCTAC
(electronic vote)
08/01/22
Review for effective date 11/01/22. Administrative
changes made to Policy Summary, Clinical Criteria,
and Applicable Coding sections. Removed coding
and criteria for voice therapy when used for the
treatment of gender dysphoria; prior authorization
requests for voice therapy must be submitted to
AIM Specialty Health as of 11/01/22.
11/01/22
Version 21
Version 21 NOT
implemented;
Version 20
effective
08/01/22 to
11/30/22
08/26/22: MPCTAC
(electronic vote)
09/01/22
Review for effective date 12/01/22. The effective
date of AIM Specialty Health’s management of
outpatient rehabilitation services changed from
11/01/22 to 12/01/22. Administrative changes
made to Policy Summary, Clinical Criteria, and
Applicable Coding sections. Removed coding and
criteria for voice therapy when used for the
treatment of gender dysphoria; prior authorization
requests for voice therapy must be submitted to
AIM for dates of service on or after 12/01/22.
12/01/22
Version 22
09/23/22: MPCTAC
(electronic vote)
Occupational Therapy in the Outpatient Setting (NH Products)
1 of 11
Medical Policy – Policy with InterQual Criteria Retired and AIM Criteria Adopted as of 12/01/22
Occupational Therapy in the Outpatient Setting
Policy Number: OCA 3.543
Version Number: 26
Policy Retired Date: 12/01/22
Impacted Products
☐ All Products
☒ NH Medicaid
☒ NH Medicare Advantage
☐ MA MassHealth ACO
☐ MA MassHealth MCO
☐ MA Qualified Health Plans/Employer Choice Direct
☐ MA Senior Care Options
Note: Disclaimer and audit information is located at the end of this document.
Policy Summary
The Plan considers outpatient occupational therapy (OT) medically necessary, including habilitative
services and/or rehabilitative services, when AIM clinical appropriateness guidelines are met for an
adult or pediatric member or are required EPSDT services for a member age 20 or younger on the date
of service. Prior authorization from AIM Specialty Health is required for outpatient OT after the initial
evaluation. OT must be provided within the scope of practice of the treating professional and/or
paraprofessional and follow all applicable state licensing and supervisory requirements.
Clinical Criteria
No medical policy criteria.
Limitations and Exclusions
None.
Variations
The Plan uses guidance from the Centers for Medicare & Medicaid Services (CMS) for medical
necessity and coverage determinations for NH Medicare Advantage members, including but not
limited to national coverage determinations (NCDs), local coverage determinations (LCDs), local
coverage articles (LCAs), and documentation included in Medicare manuals. At the time of the Plan’s
Occupational Therapy in the Outpatient Setting (NH Products)
2 of 11
most recent policy review, LCD L34427 includes medically necessary indications for occupational
therapy. Verify CMS guidelines in in effect on the date of the prior authorization request. When there
is no guidance from CMS on the requested service, Plan-adopted clinical review criteria will be used to
determine the medical necessity of the service.
Applicable Coding
The Plan utilizes up-to-date, industry-standard Current Procedural Terminology (CPT) codes, Health
Care Common Procedure Coding System (HCPCS) codes, and International Statistical Classification
of Diseases and Related Health Problems, 10th revision (ICD-10) diagnosis codes in the Plan’s medical
policies. The list of applicable codes included in this policy is informational only and may not be all
inclusive. Applicable codes are subject to change without prior notification and do not guarantee
member coverage or provider reimbursement. Review the Plan’s reimbursement policies for Plan
billing guidelines. Providers are responsible for obtaining prior authorization from AIM for occupational
therapy, even if an applicable code appropriately describing the service is not included in this policy’s
Applicable Coding section. Providers are expected to report all services using the most up-to-date,
industry-standard procedures and diagnosis codes at the time of the service.
CPT Codes
Code Descriptions
97010
Application of a modality to 1 or more areas; hot or cold packs
97012
Application of a modality to 1 or more areas; traction, mechanical
97014
Application of a modality to 1 or more areas; electrical stimulation (unattended)
97016
Application of a modality to 1 or more areas; vasopneumatic devices
97018
Application of a modality to 1 or more areas; paraffin bath
97022
Application of a modality to 1 or more areas; whirlpool
97024
Application of a modality to 1 or more areas; diathermy (e.g., microwave)
97026
Application of a modality to 1 or more areas; infrared
97028
Application of a modality to 1 or more areas; ultraviolet
97032
Application of a modality to 1 or more areas; electrical stimulation (manual), each 15 minutes
97033
Application of a modality to 1 or more areas; iontophoresis, each 15 minutes
97034
Application of a modality to 1 or more areas; contrast baths, each 15 minutes
97035
Application of a modality to 1 or more areas; ultrasound, each 15 minutes
97036
Application of a modality to 1 or more areas; Hubbard tank, each 15 minutes
97110
Therapeutic procedure, 1 or more areas, each 15 minutes; therapeutic exercises to develop
strength and endurance, range of motion and flexibility
97112
Therapeutic procedure, 1 or more areas, each 15 minutes; neuromuscular reeducation of
movement, balance, coordination, kinesthetic sense, posture, and/or proprioception for
sitting and/or standing activities
97113
Therapeutic procedure, 1 or more areas, each 15 minutes; aquatic therapy with therapeutic
exercises
97116
Therapeutic procedure, 1 or more areas, each 15 minutes; gait training (includes stair climbing)
97124
Therapeutic procedure, 1 or more areas, each 15 minutes; massage, including effleurage,
petrissage and/or tapotement (stroking, compression, percussion)
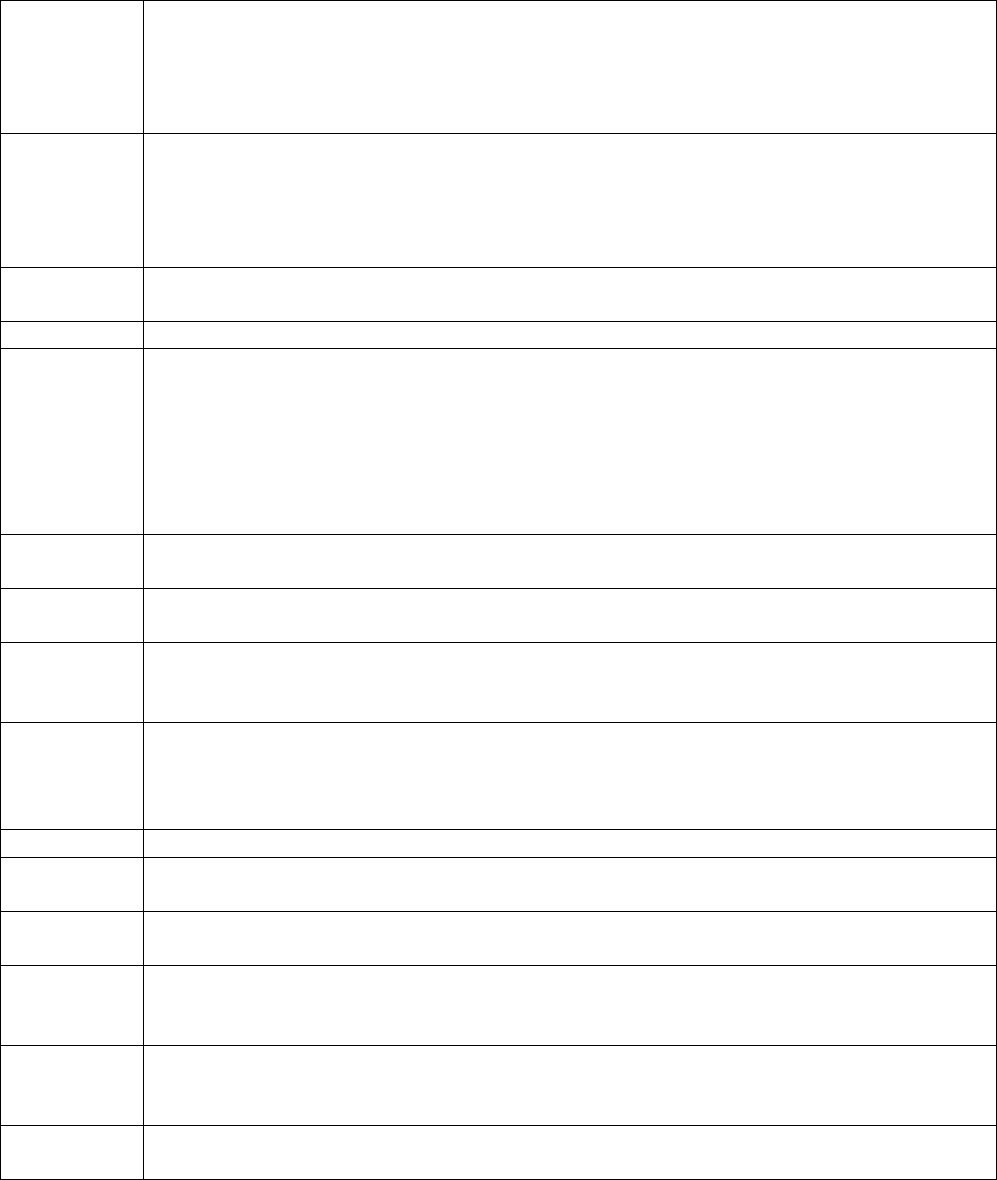
Occupational Therapy in the Outpatient Setting (NH Products)
3 of 11
97129
Therapeutic interventions that focus on cognitive function (e.g., attention, memory,
reasoning, executive function, problem solving, and/or pragmatic functioning) and
compensatory strategies to manage the performance of an activity (e.g., managing time or
schedules, initiating, organizing, and sequencing tasks), direct (one-on-one) patient contact;
initial 15 minutes
97130
Therapeutic interventions that focus on cognitive function (e.g., attention, memory,
reasoning, executive function, problem solving, and/or pragmatic functioning) and
compensatory strategies to manage the performance of an activity (e.g., managing time or
schedules, initiating, organizing, and sequencing tasks), direct (one-on-one) patient contact;
each additional 15 minutes (List separately in addition to code for primary procedure)
97140
Manual therapy techniques (e.g., mobilization/manipulation, manual lymphatic drainage,
manual traction), 1 or more regions, each 15 minutes
97150
Therapeutic procedure(s), group (2 or more individuals)
97168
Re-evaluation of occupational therapy established plan of care, requiring these components:
An assessment of changes in patient functional or medical status with revised plan of care; an
update to the initial occupational profile to reflect changes in condition or environment that
affect future interventions and/or goals; and a revised plan of care. A formal reevaluation is
performed when there is a documented change in functional status or a significant change to
the plan of care is required. Typically, 30 minutes are spent face-to-face with the patient
and/or family.
97530
Therapeutic activities, direct (one-on-one) patient contact (use of dynamic activities to
improve functional performance), each 15 minutes
97533
Sensory integrative techniques to enhance sensory processing and promote adaptive
responses to environmental demands, direct (one-on-one) patient contact, each 15 minutes
97535
Self-care/home management training (e.g., activities of daily living [ADL] and compensatory
training, meal preparation, safety procedures, and instructions in use of assistive technology
devices/adaptive equipment) direct one-on-one contact, each 15 minutes
97537
Community/work reintegration training (e.g., shopping, transportation, money management,
avocational activities and/or work environment/modification analysis, work task analysis, use
of assistive technology device/adaptive equipment), direct one-on-one contact, each 15
minutes by provider, each 15 minutes
97545
Work hardening/conditioning; initial 2 hours
97546
Work hardening/conditioning; each additional hour (List separately in addition to code for
primary procedure)
97750
Physical performance test or measurement (e.g., musculoskeletal, functional capacity), with
written report, each 15 minutes
97755
Assistive technology assessment (e.g., to restore, augment or compensate for existing
function, optimize functional tasks and/or maximize environmental accessibility), direct one-
on-one contact, with written report, each 15 minutes
97760
Orthotic(s) management and training (including assessment and fitting when not otherwise
reported), upper extremity(ies), lower extremity(ies) and/or trunk, initial orthotic(s)
encounter, each 15 minutes
97761
Prosthetic training, upper and/or lower extremity(ies), initial prosthetic(s) encounter each 15
minutes
Occupational Therapy in the Outpatient Setting (NH Products)
4 of 11
97763
Orthotic(s)/prosthetic(s) management and/or training, upper extremity(ies), lower
extremity(ies), and/or trunk, subsequent orthotic(s)/prosthetic(s) encounter, each 15
minutes
References
American Academy of Pediatrics (AAP). 2020 Recommendations for Preventive Pediatric Health Care.
Committee on Practice and Ambulatory Medicine and Bright Futures Periodicity Schedule Workgroup.
Pediatrics. 2020 Mar;145(3):e20200013. doi: 10.1542/peds.2020-0013.
American Occupational Therapy Association (AOTA). Guidelines for Supervision, Roles, and
Responsibilities During the Delivery of Occupational Therapy Services. Am J Occup Ther. 2020 Nov-
Dec;7413410020. doi: 10.5014/ajot.2020.74S3004.
American Occupational Therapy Association (AOTA). Occupational Therapy Using a Sensory
Integration-Based Approach with Adult Populations.
American Occupational Therapy Association (AOTA). Practice Guidelines.
American Occupational Therapy Association (AOTA). Scope of Practice: Questions & Answers.
Centers for Medicare & Medicaid Services (CMS). Early and Periodic Screening, Diagnostic and
Treatment (EPSDT). Medicaid.gov.
Centers for Medicare & Medicaid Services (CMS). EPSDT – A Guide for States: Coverage in the
Medicaid Benefit for Children and Adolescents. 2014 Jun.
Centers for Medicare & Medicaid Services (CMS). Local Coverage Article (LCA). Billing and Coding:
Outpatient Physical and Occupational Therapy Services A56566. 2019 Dec 19. Revision Effective Date
2020 Oct 1. National Government Services, Inc.
Centers for Medicare & Medicaid Services (CMS). Local Coverage Determination (LCD). Outpatient
Physical and Occupational Therapy Services L33631. 2015 Oct 1. Revision Effective Date 2020 Jan 1.
National Government Services, Inc.
Centers for Medicare & Medicaid Services (CMS). Manuals. Publication # 100-02. Medicare Benefit
Policy Manual.
Centers for Medicare & Medicaid Services (CMS). Manuals. Publication # 100-03. Medicare National
Coverage Determinations (NCD) Manual.
Hayes. Health Technology Assessment. Cognitive Rehabilitation Therapy for Traumatic Brain Injury
(TBI). Dallas, TX: Hayes; 2017 Sep 26. Annual Review 2021 Feb 8.
Occupational Therapy in the Outpatient Setting (NH Products)
5 of 11
Hayes. Health Technology Assessment. Occupational Therapy for Attention-Deficit/Hyperactivity
Disorder (ADHD). Dallas, TX: Hayes; 2017 Mar 16. Annual Review 2021 May 12.
New Hampshire Department of Health and Human Services. Billing Manuals.
New Hampshire Department of Health and Human Services. NH Medicaid Program.
New Hampshire Department of Health and Human Services. Provider Notices.
New Hampshire Medicaid. Therapies. Physical, Occupational, Speech. Provider Manual. Volume II. 2017
Dec 1.
New Hampshire Office of Professional Licensure and Certification. Office of Licensed Allied Health
Professionals. Laws and Administrative Rules Governing Licensed Allied Health Professionals.
Next Review Date
Not applicable
Retired Date
12/01/22
Authorizing Entity
MPCTAC
Appendix
Appendix: Policy History
Disclaimer Information:
Plan refers to Boston Medical Center Health Plan, Inc. which operates under the trade name WellSense Health Plan. Medical
Policies are the Plan’s guidelines for determining the medical necessity of certain services or supplies for purposes of
determining coverage. These Policies may also describe when a service or supply is considered experimental or
investigational, or cosmetic. In making coverage decisions, the Plan uses these guidelines and other Plan Policies, as well as
the Member’s benefit document, and when appropriate, coordinates with the Member’s health care Providers to consider the
individual Member’s health care needs.
Plan Policies are developed in accordance with applicable state and federal laws and regulations, and accrediting organization
standards (including NCQA). Medical Policies are also developed, as appropriate, with consideration of the medical necessity
definitions in various Plan products, review of current literature, consultation with practicing Providers in the Plan’s service
area who are medical experts in the particular field, and adherence to FDA and other government agency policies. Applicable
state or federal mandates, as well as the Member’s benefit document, take precedence over these guidelines. Policies are
reviewed and updated on an annual basis, or more frequently as needed. Treating providers are solely responsible for the
medical advice and treatment of Members.
Occupational Therapy in the Outpatient Setting (NH Products)
6 of 11
The use of this Policy is neither a guarantee of payment nor a final prediction of how a specific claim(s) will be adjudicated.
Reimbursement is based on many factors, including member eligibility and benefits on the date of service; medical necessity;
utilization management guidelines (when applicable); coordination of benefits; adherence with applicable Plan policies and
procedures; clinical coding criteria; claim editing logic; and the applicable Plan – Provider agreement.

Occupational Therapy in the Outpatient Setting (NH Products)
7 of 11
Appendix: Policy History
Original
Approval Date
Original Effective
Date* and Version
Policy Owner
Original Policy
Approved by
Regulatory Approval: N/A
Internal Approval:
09/16/05
10/16/05
Version 1
Director of Medical Policy as
Chair of Medical Policy,
Criteria, and Technology
Assessment Committee
(MPCTAC)
Quality and Clinical
Management
Committee
(Q&CMC)
*Effective Date for NH Medicaid Product: 01/01/13
*Effective Date for NH Medicare Advantage HMO Product: 01/01/22
Policy retired and service managed by AIM Specialty Health as of 12/01/22
Policy Revisions History
Review Date
Summary of Revisions
Revision
Effective Date
and Version
Number
Approved by
02/07/06
Added definitions for modality and visit. Defined
coverage for visits, evaluations and units billed.
Version 2
02/07/06: Q&CMC
07/06/06
Removed verbiage regarding reimbursement
for evaluation and modality services.
Version 3
07/06/06: Q&CMC
03/27/07
Policy archived.
Not applicable
Not specified
10/14/08
Policy reviewed and clinical criteria updated,
effective date of revised policy is 12/16/08.
12/16/08
Version 4
11/10/08: MPCTAC
12/16/08: Quality
Improvement
Committee (QIC)
09/22/09
No changes.
Version 5
09/22/09: MPCTAC
10/28/09: QIC
10/01/10
Updated template and references, no changes
to criteria
Version 6
10/20/10: MPCTAC
11/22/10: QIC
10/01/11
Added Commercial benefit limitations, updated
references and coding.
Version 7
10/19/11: MPCTAC
11/29/11: QIC
08/01/12
Off cycle review for the NH Medicaid product,
revised Summary statement, reformatted
Medical Policy Statement, revised Applicable
Coding introductory paragraph, updated code
list, revised limitations, deleted references to
contracts and EOCs that are not applicable.
Version 8
08/13/12: MPCTAC
09/06/12: QIC
11/01/12
Review for effective date 03/01/13. Updated
references and revised Summary section.
03/01/13
Version 9
11/21/12: MPCTAC
12/20/12: QIC
Occupational Therapy in the Outpatient Setting (NH Products)
8 of 11
Moved medical criteria from Summary section
to Clinical Guidelines Statement section.
Moved services not considered medically
necessary from the Clinical Guidelines
Statement section to the Limitations section.
Updated applicable coding list and references.
Removed duplicate text in the Clinical
Background Information section. Referenced
Plan reimbursement policy 4.609 for
occupational therapy reimbursement guidelines.
Updated language in introductory paragraph of
Applicable Coding section. Removed
“Guideline” from title.
08/14/13 and
08/15/13
Off cycle review for the NH Medicaid product
and merged policy format. Incorporate policy
revisions dated 11/01/12 (as specified above) for
the NH Medicaid product; these policy revisions
were approved by MPCTAC on 11/21/12 and QIC
on 12/20/12 for applicable Plan products.
Version 10
08/14/13: MPCTAC
(electronic vote)
08/15/13: QIC
11/01/13,
12/01/13,
01/01/14, and
02/01/14
Review for effective date 05/01/14. Updated
code definitions, introductory paragraph in
Applicable Coding section, and the applicable
code lists for the MA products and the NH
Medicaid product. Updated references.
Removed prior authorization waiver for the first
32 units of OT for the NH Medicaid product.
Add criterion in the Medical Policy Statement
sections for the MA products and NH Medicaid
product requiring an updated physician
prescription and supporting clinical
documentation after 20 OT visits per treatment
episode. Revised Limitations.
05/01/14
Version 11
02/11/14: MPCTAC
02/18/14: QIC
09/08/14
For NH Medicaid product only, waived prior
authorization of first eight (8) 15-minute
treatment units per member per servicing
provider per calendar year.
10/01/14
Version 11
Addendum A
09/17/14: MPCTAC
09/301/14: QIC
11/04/14 and
11/19/14
Review for effective date 01/11/15. Summary
and Medical Policy Statement sections updated
with guidelines specified in version 11, addendum
A. Policy renumbered OCA 3.543 to include
occupational therapy in the outpatient setting
for NH Medicaid members age 21 or older.
Summary, Limitations, and References sections
updated. (OT services formerly included in
policy number OCA 3.53 for all adult and
pediatric members.) Change in review calendar.
01/11/15
Version 12
11/06/14: MPCTAC
(electronic vote)
11/11/14: QIC
(electronic vote)
11/19/14: MPCTAC
12/10/14: QIC
Occupational Therapy in the Outpatient Setting (NH Products)
9 of 11
12/03/15
Review for effective date 01/01/16. Updated
template and Summary section. Administrative
changes made to the Medical Policy Statement
section and Limitations sections without
changing criteria. Revised language in the
Applicable Coding section. Added definitions.
01/01/16
Version 13
12/03/15: MPCTAC
(electronic vote)
12/09/15: QIC
12/01/16
Review for effective date 02/01/17. Industry-
wide revisions of applicable codes. Clarified
existing criteria in the Medical Policy Statement
section.
02/01/17
Version 14
12/21/16: MPCTAC
01/11/17: QIC
12/01/17
Review for effective 01/01/18. Industry-wide
updates to codes included in the Applicable
Coding section. Annual review of policy with
administrative changes made to the Definitions
and Reference sections.
01/01/18
Version 15
12/20/17: MPCTAC
02/01/18
Review for effective date 03/01/18.
Administrative changes made to the Policy
Summary and Limitations sections.
03/01/18
Version 16
02/21/18: MPCTAC
11/01/18
Review for effective date 12/01/18.
Administrative changes made to the Policy
Summary, Medical Policy Statement,
Limitations, Definitions, Applicable Coding,
References, Other Applicable Policies, and
Reference to Applicable Laws and Regulations
sections.
12/01/18
Version 17
11/21/18: MPCTAC
03/01/19
Review for effective date 07/01/19. Criteria and
prior authorization guidelines revised in the
Medical Policy Statement section.
Administrative changes made to the Limitations
and Reference to Applicable Laws and
Regulations sections.
07/01/19
Version 18
03/20/19: MPCTAC
12/01/19
Review for effective date 01/01/20. Industry-
wide updates to codes included in the
Applicable Coding section.
01/01/20
Version 19
Not applicable because
industry-wide code
changes
11/01/19
Review for effective date 02/01/20. Revised
criteria in the Medical Policy Statement and
Limitations sections. Administrative changes
made to the References Reference to
Applicable Laws and Regulations sections.
02/01/20
Version 20
Renumbered to
version 20 to
implement
industry-wide
code updates
effective
01/01/20 in
version 19
11/20/19: MPCTAC
Occupational Therapy in the Outpatient Setting (NH Products)
10 of 11
12/01/19
Review for effective 02/01/20. Industry-wide
updates to codes effective 01/01/20 included in
the Applicable Coding section of the policy
version 20 effective 02/01/20.
02/01/20
Version 21
Not applicable because
industry-wide code
changes
12/01/19
Review for effective date 03/01/20. Revised in
the Medical Policy Statement section the
definition of a servicing OT provider for the
prior authorization waiver.
03/01/20
Version 22
12/18/19: MPCTAC
11/01/20
Review for effective date 12/01/20. Updated
the References section. Administrative change
made to the Applicable Coding section.
12/01/20
Version 23
11/18/20: MPCTAC
11/01/21
Review for effective date 12/01/21. Adopted
new medical policy template; removed
administrative sections, Medical Policy
Statement section renamed Clinical Criteria
section, and Limitations section renamed
Limitations and Exclusions section. Added NH
Medicare Advantage HMO as an applicable
product effective 01/01/22. Administrative
changes made to the Policy Summary and
References sections. Criteria revised in the
Clinical Criteria and Limitations and Exclusions
sections. Medical policy criteria retired and
InterQual criteria will continue to be used to
determine medical necessity.
12/01/21
Version 24
11/17/21: MPCTAC
08/01/22
Review for effective date 11/01/22.
Administrative changes made to the Policy
Summary and Applicable Coding sections.
InterQual medical necessity criteria and medical
policy guidelines in the Clinical Criteria and
Limitations and Exclusions sections retired on
11/01/22. AIM criteria adopted for outpatient
OT on 11/01/22. Plan prior authorization waivers
removed after 10/31/22. AIM prior authorization
is required for outpatient OT after the initial
evaluation as of 11/01/22, even when applicable
codes are not listed in this Plan policy.
11/01/22
Version 25
Version 25 NOT
implemented;
Version 24
effective
12/01/21 to
11/30/22
08/26/22: MPCTAC
(electronic vote)
09/01/22
Review for policy retired date 12/01/22. The
effective date of AIM Specialty Health’s
management of outpatient rehabilitation
services changed from 11/01/22 to 12/01/22.
Administrative changes made to the Policy
Summary and Applicable Coding sections.
InterQual medical necessity criteria and medical
policy guidelines in the Clinical Criteria and
Limitations and Exclusions sections retired on
12/01/22
Version 26
09/23/22: MPCTAC
(electronic vote)
Occupational Therapy in the Outpatient Setting (NH Products)
11 of 11
12/01/22. AIM criteria adopted for outpatient
OT for dates of service on or after 12/01/22.
Plan prior authorization waivers removed after
11/30/22. AIM prior authorization is required for
outpatient OT after the initial evaluation as of
12/01/22, even when applicable codes are not
listed in this Plan policy.
Pelvic Floor Stimulation for the Treatment of Incontinence and/or Overactive Bladder
1 of 14
Medical Policy – Policy Retired and AIM Criteria Adopted as of 12/01/22
Pelvic Floor Stimulation for the Treatment of Incontinence and/or
Overactive Bladder
Policy Number: OCA 3.561
Version Number: 26
Policy Retired Date: 12/01/22
Impacted Products
☒ All Products
☒ NH Medicaid
☒ NH Medicare Advantage
☒ MA MassHealth ACO
☒ MA MassHealth MCO
☒ MA Qualified Health Plans/Employer Choice Direct
☒ MA Senior Care Options
Note: Disclaimer and audit information is located at the end of this document.
Policy Summary
AIM Specialty Health’s clinical appropriateness criteria will be used to determine if non-implantable
pelvic floor stimulation is considered medically necessary for the treatment of overactive bladder,
urinary incontinence and/or fecal incontinence; this includes pelvic floor electrical stimulation (PFES)
and/or pelvic floor magnetic stimulation. Prior authorization from AIM is required.
Clinical Criteria
No medical policy criteria.
Limitations and Exclusions
None.
Variations
The Plan uses guidance from the Centers for Medicare & Medicaid Services (CMS) for medical
necessity and coverage determinations for Senior Care Options (SCO) members and NH Medicare
Advantage HMO members, including but not limited to national coverage determinations (NCDs), local
coverage determinations (LCDs), local coverage articles (LCAs), and documentation included in
Medicare manuals. At the time of the Plan’s most recent policy review, CMS NCD 230.8 8 includes
medically necessary indications for the use of a non-implantable pelvic floor electrical stimulator. No
Pelvic Floor Stimulation for the Treatment of Incontinence and/or Overactive Bladder
2 of 14
CMS clinical criteria were identified for pelvic floor magnetic stimulation for urinary incontinence or
fecal incontinence or the use of pelvic floor electrical stimulation (PFES) for fecal incontinence. Verify
CMS guidelines in effect on the date of the prior authorization request. When there is no guidance
from CMS for the requested service, Plan-adopted clinical review criteria will be used to determine the
medical necessity of the service.
Applicable Coding
The Plan utilizes up-to-date, industry-standard Current Procedural Terminology (CPT) codes, Health
Care Common Procedure Coding System (HCPCS) codes, and International Statistical Classification
of Diseases and Related Health Problems, 10th revision (ICD-10) diagnosis codes in the Plan’s medical
policies. The list of applicable codes included in a policy is informational only and may not be all
inclusive. Applicable codes are subject to change without prior notification and do not guarantee
member coverage or provider reimbursement. Review the Plan’s reimbursement policies for Plan
billing guidelines. Providers are responsible for obtaining prior authorization for this services, even if an
applicable code appropriately describing the service is not included in this policy’s Applicable Coding
section. Providers are expected to report all services using the most up-to-date, industry-standard
procedures and diagnosis codes at the time of the service.
CPT/HCPCS Codes
Code Descriptions
97014
Application of a modality to 1 or more areas; electrical stimulation (unattended)
Note: Supervised. The application of a modality that does not require direct, one-
on-one, patient contact by the provider.
Plan note: Code is NOT payable for the Senior Care Options and NH Medicare
Advantage HMO products.
97032
Application of a modality to 1 or more areas; electrical stimulation (manual), each 15
minutes
E0740
Non-implanted pelvic floor electrical stimulator, complete system
G0283
Electrical stimulation (unattended), to one or more areas for indication(s) other than
wound care, as part of a therapy plan of care
References
Abdelbary AM, El-Dessoukey AA, Massoud AM, Moussa AS, Zayed AS, Elsheikh MG, Ghoneima W,
Abdella R, Yousef M. Combined Vaginal Pelvic Floor Electrical Stimulation (PFS) and Local Vaginal
Estrogen for Treatment of Overactive Bladder (OAB) in Perimenopausal Females. Randomized
Controlled Trial (RCT). Urology. 2015 Sep;86(3):482-6. doi: 10.1016/j.urology.2015.06.007. Epub 2015
Jun 30. PMID: 26135813.
Abrams P, Andersson KE, Birder L, Brubaker L, Cardozo L, Chapple C, Cottenden A, Davila W, de
Ridder D, Dmochowski R, Drake M, Dubeau C, Fry C, Hanno P, Smith JH, Herschorn S, Hosker
G, Kelleher C, Koelbl H, Khoury S, Madoff R, Milsom I, Moore K, Newman D, Nitti V, Norton C, Nygaard
I, Payne C, Smith A, Staskin D, Tekgul S, Thuroff J, Tubaro A, Vodusek D, Wein A, Wyndaele
JJ; Members of Committees; Fourth International Consultation on Incontinence. Fourth international
Pelvic Floor Stimulation for the Treatment of Incontinence and/or Overactive Bladder
3 of 14
consultation on incontinence recommendations of the International Scientific Committee: Evaluation
and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol
Urodyn. 2010;29(1):213-40. doi: 10.1002/nau.20870. PMID: 20025020.
American College of Gastroenterology (ACG). Guidelines.
The American College of Obstetricians and Gynecologists (ACOG). Clinical Guidance.
The American College of Obstetricians and Gynecologists (ACOG). ACOG Practice Bulletin No. 155.
Urinary Incontinence in Women. 2015. Reaffirmed 2018. Obstet Gynecol. 2015 Nov;126(5):e66-81. doi:
10.1097/AOG.0000000000001148. PMID: 26488524.
The American College of Obstetricians and Gynecologists (ACOG). ACOG Practice Bulletin No. 210.
Fecal Incontinence. Obstet Gynecol. 2019 Apr;133(4):837-39. doi: 10.1097/
AOG.0000000000003188. PMID: 30913191.
The American College of Obstetricians and Gynecologists (ACOG), American Urogynecologic Society
(AUGS). ACOG Committee on Gynecologic Practice. Evaluation of Uncomplicated Stress Urinary
Incontinence in Women Before Surgical Treatment. Committee Opinion Number 603. 2014 Jun.
Reaffirmed 2017.
The American College of Obstetricians and Gynecologists (ACOG). Urinary Incontinence. Patient
Resources.
American College of Physicians (ACP). Clinical Guidelines & Recommendations.
American College of Physicians (ACP). Qaseem A, Dallas P, Forciea MA, Starkey M, Denberg TD,
Shekelle P. Clinical Guidelines Committee of the ACP. Nonsurgical management of urinary
incontinence in women: a clinical practice guideline from the ACP. Ann Intern Med. 2014 Sep
16;161(6):429-40. doi: 10.7326/M13-2410. PMID: 25222388.
American Gastroenterological Association (AGA). Bharucha AE, Pemberton JH, Locke GR. American
Gastroenterological Association technical review on constipation. Gastroenterology. 2013
Jan;144(1):218-38. doi: 10.1053/j.gastro.2012.10.028. PMID: 23261065.
American Gastroenterological Association (AGA). Clinical Guidelines.
American Society of Colon and Rectal Surgeons (ASCRS). Paquette IM, Varma MG, Kaiser AM, Steele
SR, Rafferty JF. The ASCRS' Clinical Practice Guideline for the Treatment of Fecal Incontinence. Dis
Colon Rectum. 2015 Jul;58(7):623-36. doi: 10.1097/DCR.0000000000000397. PMID: 26200676.
American Society of Colon and Rectal Surgeons (ASCRS). Paquette IM, Varma M, Ternent C, Melton-
Meaux G, Rafferty J, Feingold D, Steele SR. The ASCRS’ Clinical Practice Guideline for the Evaluation
Pelvic Floor Stimulation for the Treatment of Incontinence and/or Overactive Bladder
4 of 14
and Management of Constipation. Dis Colon Rectum 2016; 59: 479–92. doi: 10.1097/
DCR.0000000000000599. PMID: 27145304.
American Urogynecologic Society (AUGS). Clinical Guidance Documents.
American Urological Association (AUA). Guidelines & Policies.
American Urological Association (AUA) and Society of Urodynamics, Female Pelvic Medicine &
Urogenital Reconstruction (SUFU). Lightner DJ, Gomelsky A, Souter L, Vasavada SP. Diagnosis and
Treatment of Overactive Bladder (Non-Neurogenic) in Adults: AUA/SUFU Guideline Amendment
2019. J Urol. 2019 Sep;202(3):558-63. doi: 10.1097/JU.0000000000000309. Epub 2019 Aug 8.
PMID: 31039103.
Anderson CA, Omar MI, Campbell SE, Hunter KF, Cody JD, Glazener CM. Conservative management
for postprostatectomy urinary incontinence. Cochrane Database Syst Rev. 2015 Jan 20;1:CD001843.
doi: 10.1002/14651858.CD001843.pub5. PMID: 25602133.
Aydin S, Arioglu Aydin Ç, Batmaz G, Dansuk R. Effect of vaginal electrical stimulation on female sexual
functions: a randomized study. J Sex Med. 2015 Feb;12(2):463-9. doi: 10.1111/jsm.12788. Epub 2014 Dec
3. PMID: 25470078.
Berghmans B, Hendriks E, Bernards A, de Bie R, Omar MI. Electrical stimulation with non-implanted
electrodes for urinary incontinence in men. Cochrane Database Syst Rev. 2013 Jun 6;(6):CD001202.
doi: 10.1002/14651858.CD001202.pub5. PMID: 23740763.
Canadian Urological Association. Bettez M, Tu LM, Carlson K, Corcos J, Gajewski J, Jolivet M, Bailly G.
2012 Update: Guidelines for Adult Urinary Incontinence Collaborative Consensus Document for the
Canadian Urological Association. Can Urol Assoc J. 2012 Oct;6(5):354–63. doi: 10.5489/cuaj.12248.
PMID: 23093627.
Centers for Medicare & Medicaid Services (CMS). Local Coverage Determination (LCD) Posterior
Tibial Nerve Stimulation for Voiding Dysfunction L33396. National Government Services, Inc. 2015 Oct
1. Revision Effective Date 2019 Oct 24.
Centers for Medicare & Medicaid Services (CMS). Manuals. Publication # 100-02. Medicare Benefit
Policy Manual.
Centers for Medicare & Medicaid Services (CMS). Manuals. Publication # 100-03. Medicare National
Coverage Determinations (NCD) Manual.
Centers for Medicare & Medicaid Services (CMS). Medicare Coverage Database (MCD).
Centers for Medicare & Medicaid Services (CMS). National Coverage Determination (NCD) for
Biofeedback Therapy for the Treatment of Urinary Incontinence 30.1.1. Effective 2001 Jul 1.
Pelvic Floor Stimulation for the Treatment of Incontinence and/or Overactive Bladder
5 of 14
Centers for Medicare & Medicaid Services (CMS). National Coverage Determination (NCD) for
Bladder Stimulators (Pacemakers) 230.16. 1996 Oct 7.
Centers for Medicare & Medicaid Services (CMS). National Coverage Determination (NCD) for Non-
Implantable Pelvic Floor Electrical Stimulator 230.8. Effective 2006 Jun 19.
Centers for Medicare & Medicaid Services (CMS). National Coverage Determination (NCD) for Sacral
Nerve Stimulation for Urinary Incontinence (230.18). Effective 2002 Jan 1.
Centers for Medicare & Medicaid Services (CMS). Transmittals.
Chêne G, Mansoor A, Jacquetin B, Mellier G, Douvier S, Sergent F, Aubard Y, Seffert P. Female urinary
incontinence and intravaginal electrical stimulation: an observational prospective study. Eur J Obstet
Gynecol Reprod Biol. 2013 Sep;170(1):275-80. doi: 10.1016/j.ejogrb.2013.06.011. Epub 2013 Jul 5. PMID:
23830965.
Chughtai B, Lee R, Sandhu J, Te A, Kaplan S. Conservative Treatment for Postprostatectomy
Incontinence. Rev Urol. 2013;15(2):61–6. PMID: 24082844.
Commonwealth of Massachusetts. Division of Insurance (DOI) Bulletins.
Commonwealth of Massachusetts. MassHealth Provider Bulletins.
Commonwealth of Massachusetts. MassHealth Provider Manuals.
Commonwealth of Massachusetts. MassHealth Transmittal Letters.
Correia, GN, Pereira, VS, Hirakawa, HS, Driusso, P. Effects of surface and intravaginal electrical
stimulation in the treatment of women with stress urinary incontinence: randomized controlled trial. Eur
J Obstet Gynecol Reprod Biol. 2014 Feb;173:113-8. doi: 10.1016/j.ejogrb.2013.11.023. Epub 2013 Dec 4.
PMID: 24382548.
Dumoulin C, Hay-Smith EJC, Mac Habée-Séguin G. Pelvic floor muscle training versus no treatment,
or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev. 2014
May 14;(5):CD005654. doi: 10.1002/14651858.CD005654.pub3. PMID: 24823491.
European Association of Urology (EAU). Blok B, Castro-Diaz D, Del Popolo G, Groen J, Hamid R,
Karsenty G, Kessler TM, Pannek J, Ecclestone H, Musco S, Padilla-Fernández B, Sartori A, 't Hoen LA.
EAU Guidelines. Neuro-Urology. 2020 Mar. Edn. presented at the EAU Annual Congress Amsterdam
2022. ISBN 978-94-92671-16-5.
European Association of Urology (EAU). Gacci M, Sakalis VI, Karavitakis M, Cornu JN, Gratzke C,
Hermann TRW, Kyriazis I, Malde S, Mamoulakis C, Rieken M, Schouten N, Smith EJ, Speakman MJ,

Pelvic Floor Stimulation for the Treatment of Incontinence and/or Overactive Bladder
6 of 14
Tikkinen KAO, Gravas S. EAU Guidelines on Male Urinary Incontinence. Rev Incon. 2022 Oct
1;82(4):387-98. doi: 10.1016/j.euro.2022.05.0122.
European Association of Urology (EAU). Nambiar AK, Arlandis S, Bo K, Cobussen-Boekhorst H,
Costantini E, de Heide M, Farag F, Groen J, Karavitakis M, Lapitan MC, Manso M, Monagas Arteaga S,
Nic An Riogh A, O’Connor E, Omar MI, Peyronnet B, Phe V, Sakalis VI, Sihra N, Tzelves L, van
Poelgeest-Pomfret ML, van den Bos TWL, van der Vaart H, Harding CK. EAU Guidelines on the
Diagnosis and Management of Female Non-Neurogenic Lower Urinary Tract Symptoms. Part 1:
Diagnostics, Overactive Bladder, Stress Urinary Incontinence, and Mixed Urinary Incontinence.
European Urology. 2022 Jul;82(1):60-70. doi: 10.1016/j.eururo.2022.01.045.
European Association of Urology (EAU). Nambiar AK, Bosch R, Cruz F, Lemack GE, Thiruchelvam N,
Tubaro A, Bedretdinova DA, Ambühl D, Farag F, Lombardo R, Schneider MP, Burkhard FC. EAU
Guidelines on Assessment and Nonsurgical Management of Urinary Incontinence. Eur Urol. 2018
Apr;73(4):596-609. doi: 10.1016/j.eururo.2017.12.031. Epub 2018 Feb 3.PMID: 29398262.
European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN), North
American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN). Tabbers
MM, DiLorenzo C, Berger MY, Faure BC, Langendam MW, Nurko S, Staiano A, Vandenplas Y, Benninga
MA. Clinical Guideline. Evaluation and Treatment of Functional Constipation in Infants and Children:
Evidence-Based Recommendations from ESPGHAN and NASPGHAN. J Pediatr Gastroenterol
Nutr. 2014 Feb;58(2):258-74. doi: 10.1097/MPG.0000000000000266. PMID: 24345831.
Faiena I, Patel N, Parihar JS, Calabrese M, Tunuguntla H. Conservative Management of Urinary
Incontinence in Women. Rev Urol. 2015;17(3):129–39. PMID: 26543427.
Fernández-Cuadros ME, Nieto-Blasco J, Geanini-Yagüez A, Ciprián-Nieto D, Padilla-Fernández B,
Lorenzo-Gómez MF. Male Urinary Incontinence: Associated Risk Factors and Electromyography
Biofeedback Results in Quality of Life. Am J Mens Health. 2016 Nov;10(6):NP127-35. Epub 2015 Jun
30. doi: 10.1177/1557988315590653. PMID: 26130728.
Fritel X, Fauconnier A, Bader G, Cosson M, Debodinance P, Deffieux X, Denys P, Dompeyre P, Faltin
D, Fatton B, Haab F, Hermieux JF, Kerdraon J, Mares P, Mellier G, Michel-Laaengh N, Nadeau
C, Robain G, de Tayrac R, Jacquetin B; French College of Gynecologists and Obstetricians. Diagnosis
and management of adult female stress urinary incontinence: guidelines for clinical practice from the
French College of Gynecologists and Obstetricians. Eur J Obstet Gynecol Reprod Biol. 2010
Jul;151(1):14-9. doi: 10.1016/j.ejogrb.2010.02.041. Epub 2010 Mar 16. PMID: 20236751.
Fürst MC, Mendonça RR, Rodrigues AO, Matos LL, Pompeo AC, Bezerra CA. Long-term results of a
clinical trial comparing isolated vaginal stimulation with combined treatment for women with stress
incontinence. Einstein (Sao Paulo). 2014 Apr;12(2):168-74. doi: 10.1590/s1679-45082014ao2866.
PMID: 25003921.

Pelvic Floor Stimulation for the Treatment of Incontinence and/or Overactive Bladder
7 of 14
Ghaderi F, Oskouei AE. Physiotherapy for Women with Stress Urinary Incontinence: A Review Article. J
Phys Ther Sci. 2014 Sep;26(9):1493–9. doi: 10.1589/jpts.26.1493. Epub 2014 Sep 17. PMID: 25276044.
Gilling PJ, Wilson LC, Westenberg AM, McAllister WJ, Kennett KM, Frampton CM, Bell DF, Wrigley
PM, Fraundorfer MR. A double-blind randomized controlled trial of electromagnetic stimulation of the
pelvic floor vs. sham therapy in the treatment of women with stress urinary incontinence. BJU Int. 2009
May;103(10):1386-90. Epub 2009 Jan 14. doi: 10.1111/j.1464-410X.2008.08329.x. Epub 2009 Jan 14.
PMID: 19154474.
Goode PS, Burgio KL, Johnson TM 2nd, Clay OJ, Roth DL, Markland AD, Burkhardt JH, Issa MM, Lloyd
LK. Behavioral therapy with or without biofeedback and pelvic floor electrical stimulation for persistent
postprostatectomy incontinence: a randomized controlled trial. JAMA. 2011 Jan 12;305(2):151-9. doi:
10.1001/jama.2010.1972. PMID: 21224456.
Gungor Ugurlucan F, Onal M, Aslan E, Ayyildiz Erkan H, Kizilkaya Beji N, Yalcin O. Comparison of the
effects of electrical stimulation and posterior tibial nerve stimulation in the treatment of overactive
bladder syndrome. Gynecol Obstet Invest. 2013;75(1):46-52. doi: 10.1159/000343756. Epub 2012 Nov
16. PMID: 23171636.
Guralnick ML, Kelly H, Engelke H, Koduri S, O'Connor RC. InTone: a novel pelvic floor rehabilitation
device for urinary incontinence. Int Urogynecol J. 2015 Jan;26(1):99-106. doi: 10.1007/s00192-014-
2476-9. Epub 2014 Jul 30. PMID: 25074260.
Hersh L, Salzman B. Clinical management of urinary incontinence in women. Am Fam Physician. 2013
May;87(9):634-40. Erratum in: Am Fam Physician. 2013 May 1;87(9):634-40. PMID: 23668526.
International Urogynecological Association (IUGA), International Continence Society (ICS). Haylen BT,
de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, Monga A, Petri E, Rizk DE, Sand PK, Schaer
GN. An IUGA/ICS joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol
J. 2010 Jan;21(1):5-26. doi: 10.1007/s00192-009-0976-9. Epub 2009 Nov 25. PMID: 19937315.
Joussain C, Denys P. Electrical management of neurogenic lower urinary tract disorders. Ann Phys
Rehabil Med. 2015 Sep;58(4):245-250. doi: 10.1016/j.rehab.2015.07.005. Epub 2015 Aug 25. PMID:
26321622.
Lim R, Liong ML, Leong WS, Khan NA, Yuen KH. Magnetic stimulation for stress urinary incontinence:
study protocol for a randomized controlled trial. Trials. 2015 Jun 21;16:279. doi: 10.1186/s13063-015-
0803-1. PMID: 26093910.
Maher RM, Caulfield B. A novel externally applied neuromuscular stimulator for the treatment of stress
urinary incontinence in women-a pilot study. Neuromodulation. 2013 Nov-Dec;16(6):590-4; discussion
594. doi: 10.1111/j.1525-1403.2012.00509.x. Epub 2012 Sep 25. PMID: 23009698.
Pelvic Floor Stimulation for the Treatment of Incontinence and/or Overactive Bladder
8 of 14
Mariotti G, Salciccia S, Innocenzi M, Gentilucci A, Fasulo A, Gentile V, Sciarra A. Recovery of Urinary
Continence After Radical Prostatectomy Using Early vs. Late Pelvic Floor Electrical Stimulation and
Biofeedback-associated Treatment. Urology. 2015 Jul;86(1):115-20. doi: 10.1016/j.urology.2015.02.064.
PMID: 26142594.
Maternik M, Krzeminska K, Zurowska A. The management of childhood urinary incontinence. Pediatr
Nephrol. 2015 Jan;30(1):41-50. doi: 10.1007/s00467-014-2791-x. Epub 2014 Mar 11. PMID: 24615564.
Morin F, Akhavizadegan H, Kavanagh A, Moore K. Dysfunctional voiding: Challenges of disease
transition from childhood to adulthood. Can Urol Assoc J. 2018 Apr;12(4 Suppl 1):S42-7. doi:
10.5489/cuaj.5230. PMID: 29681274.
Moroni RM, Magnani PS, Haddad JM, Castro Rde A, Brito LG. Conservative Treatment of Stress
Urinary Incontinence: A Systematic Review with Meta-analysis of Randomized Controlled Trials. Rev
Bras Ginecol Obstet. 2016 Feb;38(2):97-111. doi: 10.1055/s-0035-1571252. Epub 2016 Jan 29. PMID:
26883864.
National Institute for Health and Care Excellence (NICE). Lower urinary tract symptoms in men:
management. Clinical Guideline CG97. 2010 May 23. Last Updated 2015 Jun 3.
National Institute for Health and Care Excellence (NICE). Urinary incontinence in neurological disease:
assessment and management. Clinical Guideline CG148. 2012 Aug 8.
National Institute for Health and Care Excellence (NICE). Urinary incontinence and pelvic organ
prolapse in women: management. NICE Guideline NG123. 2019 Apr 2. Last Updated 2019 Jun 24.
Nepple KG, Cooper CS. Management of bladder dysfunction in children. UpToDate. 2021 Jun 22.
New Hampshire Department of Health and Human Services. Billing Manuals.
New Hampshire Department of Health and Human Services. Provider Notices.
Santos JD, Lopes RI, Koyle MA. Bladder and bowel dysfunction in children: An update on the diagnosis
and treatment of a common, but underdiagnosed pediatric problem. Can Urol Assoc J. 2017 Jan-
Feb;11(1-2Suppl1):S64-72. doi: 10.5489/cuaj.4411. PMID: 28265323.
Schreiner L, Santos TG, Souza AB, Nygaard CC, Silva Filho IG. Electrical stimulation for urinary
incontinence in women: a systematic review. Int Braz J Urol. 2013 Jul-Aug;39(4):454-64. doi:
10.1590/S1677-5538.IBJU.2013.04.02. PMID: 24054395.
Terlikowski R, Dobrzycka B, Kinalski M, Kuryliszyn-Moskal A, Terlikowski SJ. Transvaginal electrical
stimulation with surface-EMG biofeedback in managing stress urinary incontinence in women of
premenopausal age: a double-blind, placebo-controlled, randomized clinical trial. Int Urogynecol J.
2013 Oct;24(10):1631-8. doi: 10.1007/s00192-013-2071-5. Epub 2013 Feb 27. PMID: 23443345.
Pelvic Floor Stimulation for the Treatment of Incontinence and/or Overactive Bladder
9 of 14
Tugtepe H, Thomas DT, Ergun R, Kalyoncu A, Kaynak A, Kastarli C, Dagli TE. The effectiveness of
transcutaneous electrical neural stimulation therapy in patients with urinary incontinence resistant to
initial medical treatment or biofeedback. J Pediatr Urol. 2015 Jun;11(3):137.e1-5. doi:
10.1016/j.jpurol.2014.10.016. Epub 2015 Mar 12. PMID: 25824876.
U.S. Food and Drug Administration (FDA). Clinical Investigations of Devices Indicated for the
Treatment of Urinary Incontinence – Guidance for Industry and FDA Staff. 2011 Mar 8.
U. S. Food and Drug Administration (FDA). Medical Devices. 510(k) Clearances.
U. S. Food and Drug Administration (FDA). Medical Devices. Device Registration and Listing.
Wald A. Diagnosis and Management of Fecal Incontinence. Curr Gastroenterol Rep. 2018 Mar
26;20(3):9. doi: 10.1007/s11894-018-0614-0. PMID: 29582182.
Wallis MC, Davies EA, Thalib L, Griffiths S. Pelvic static magnetic stimulation to control urinary
incontinence in older women: a randomized controlled trial. Clin Med Res. 2012 Feb;10(1):7-14. doi:
10.3121/cmr.2011.1008. Epub 2011 Aug 4. PMID: 21817123.
Yamanishi T, Mizuno T, Watanabe M, Honda M, Yoshida K. Randomized, placebo controlled study of
electrical stimulation with pelvic floor muscle training for severe urinary incontinence after radical
prostatectomy. J Urol. 2010 Nov;184(5):2007-12. doi: 10.1016/j.juro.2010.06.103. Epub 2010 Sep 20.
PMID: 20850831.
Zhu YP, Yao XD, Zhang SL, Dai B, Ye DW. Pelvic floor electrical stimulation for postprostatectomy
urinary incontinence: a meta-analysis. Urology 2012 Mar;79(3):552-5. doi: 10.1016/
j.urology.2011.10.005. PMID: 22386394.
Next Review Date
Not applicable
Retired Date
12/01/22
Authorizing Entity
MPCTAC
Appendix
Appendix: Policy History
Pelvic Floor Stimulation for the Treatment of Incontinence and/or Overactive Bladder
10 of 14
Disclaimer Information:
Plan refers to Boston Medical Center Health Plan, Inc. which operates under the trade name WellSense Health Plan. Medical
Policies are the Plan’s guidelines for determining the medical necessity of certain services or supplies for purposes of
determining coverage. These Policies may also describe when a service or supply is considered experimental or
investigational, or cosmetic. In making coverage decisions, the Plan uses these guidelines and other Plan Policies, as well as
the Member’s benefit document, and when appropriate, coordinates with the Member’s health care Providers to consider the
individual Member’s health care needs.
Plan Policies are developed in accordance with applicable state and federal laws and regulations, and accrediting organization
standards (including NCQA). Medical Policies are also developed, as appropriate, with consideration of the medical necessity
definitions in various Plan products, review of current literature, consultation with practicing Providers in the Plan’s service
area who are medical experts in the particular field, and adherence to FDA and other government agency policies. Applicable
state or federal mandates, as well as the Member’s benefit document, take precedence over these guidelines. Policies are
reviewed and updated on an annual basis, or more frequently as needed. Treating providers are solely responsible for the
medical advice and treatment of Members.
The use of this Policy is neither a guarantee of payment nor a final prediction of how a specific claim(s) will be adjudicated.
Reimbursement is based on many factors, including member eligibility and benefits on the date of service; medical necessity;
utilization management guidelines (when applicable); coordination of benefits; adherence with applicable Plan policies and
procedures; clinical coding criteria; claim editing logic; and the applicable Plan – Provider agreement.

Pelvic Floor Stimulation for the Treatment of Incontinence and/or Overactive Bladder
11 of 14
Appendix: Policy History
Original
Approval Date
Original Effective
Date and Version
Policy Owner
Original Policy
Approved by
Regulatory Approval: N/A
Internal Approval:
10/03/06
12/03/06
Version 1
Director of Medical Policy as
Chair of Medical Policy,
Criteria, and Technology
Assessment Committee
(MPCTAC)
Quality and Clinical
Management
Committee
(Q&CMC)
*Effective Date for QHP Commercial Product: 01/01/12
*Effective Date for New Hampshire Medicaid Product: 01/01/13
*Effective Date for Senior Care Options Product: 01/01/16
*Effective Date for New Hampshire Medicare Advantage HMO Product: 01/01/22
This policy replaced Pelvic Floor/Sacral Nerve Stimulation for Urinary Incontinence medical policy, policy number
OCA 3.56, as of 05/01/13 for criteria related to pelvic floor stimulation for the treatment of incontinence. The
policy was titled Non-Implantable Pelvic Floor Electrical Stimulation for Urinary Incontinence from 05/01/13 to
01/31/16. The policy title was Pelvic Floor Stimulation for the Treatment of Incontinence from 02/01/16 to
02/28/19. Effective 03/01/19, the policy title has been changed to Pelvic Floor Stimulation for the Treatment of
Incontinence and/or Overactive Bladder. Policy retired and service managed by AIM Specialty Health as of
12/01/22.
Policy Revisions History
Review
Date
Summary of Revisions
Revision Effective
Date and Version
Number
Approved by
09/11/07
Updated template, added coding, approved by
MPCTAC.
Version 2
09/11/07: MPCTAC
09/25/07: Utilization
Management
Committee (UMC)
10/15/07: Quality
Improvement
Committee (QIC)
09/09/08
No changes.
Version 3
09/09/08: MPCTAC
09/30/08: UMC
10/22/08: QIC
09/22/09
Updated references, no changes to criteria.
Version 4
09/22/09: MPCTAC
10/28/09: QIC
09/01/10
Updated template and references, no changes
to criteria.
Version 5
10/20/10: MPCTAC
11/22/10: QIC
10/01/11
Updated limitations to include that sacral nerve
stimulation for the treatment of fecal
incontinence and posterior tibial nerve
stimulation for the treatment of symptoms
Version 6
10/19/11: MPCTAC
11/29/11: QIC
Pelvic Floor Stimulation for the Treatment of Incontinence and/or Overactive Bladder
12 of 14
associated with overactive bladder are
considered experimental and investigational.
Updated references and coding.
07/20/12
Off cycle review for Well Sense Health Plan:
Updated title, revised Summary statement,
added posterior tibial stimulation to Description
of Item or Service, reformatted Medical Policy
Statement, updated Definitions, revised
language in Applicable Coding section, updated
code list.
Version 7
08/13/12: MPCTAC
09/13/12: QIC
12/01/12
Separated pelvic floor electrical stimulation,
sacral nerve stimulation, and posterior tibial
nerve stimulation into three separate policies;
policy formerly titled Pelvic Floor/Sacral Nerve
Stimulation for Urinary Incontinence (formerly
policy number OCA: 3.65). Revised title and re-
numbered policy. Updated language in
Summary, Description of Item or Service,
Definitions, Applicable Coding, and Clinical
Background Information sections. Referenced
Posterior Tibial Nerve Stimulation, Sacral Nerve
Stimulation (Including Peripheral Nerve
Stimulation Test and Two-Stage Tined Lead
Procedure) for Incontinence and Urinary
Conditions, Biofeedback for Urinary
Incontinence, Experimental and Investigation
Treatment, and Medically Necessary policies.
Reformatted and added criteria in Medical
Policy Statement section, updated and added
references, and added limitations. Revised
applicable code list.
Version 8
12/19/12: MPCTAC
01/31/13: QIC
12/01/13
Review for effective date 02/01/14. Updated
references.
02/01/14
Version 9
12/18/13: MPCTAC
01/21/14: QIC
12/01/14
Review for effective date 05/01/15. Updated
references. Added ICD9/ICD10 diagnosis codes
for urinary incontinence to the Applicable
Coding section. Updated introductory
paragraph in the Applicable Coding section.
05/01/15
Version 10
12/17/14: MPCTAC
01/14/15: QIC
10/01/15
Review for effective date 12/01/15. Updated
template with list of applicable products and
corresponding notes.
12/01/15
Version 11
10/21/15: MPCTAC
11/11/15: QIC
10/21/15
Review for effective date 02/01/16. Updated
Summary, Description of Item or Service,
Definitions, Clinical Background Information,
and References sections. Updated criteria in the
Medical Policy Statement and Limitations
sections. Revised the title of the policy.
02/01/16
Version 12
10/21/15: MPCTAC
11/11/15: QIC
Pelvic Floor Stimulation for the Treatment of Incontinence and/or Overactive Bladder
13 of 14
11/25/15
Review for effective date 02/01/16. Revised
language in the Applicable Coding section. Plan
note added to HCPCS code G0283.
02/01/16
Version 13
11/25/15: MPCTAC
(electronic vote)
12/09/15: QIC
10/01/16
Review for effective date 12/01/16. Updated
Summary, Definitions, Clinical Background
Information, References, and References to
Applicable Laws and Regulations sections.
Administrative changes made to the Medical
Policy Statement and Limitations sections; no
change to criteria. Removed ICD-9 diagnosis
codes and Plan notes added to applicable
codes.
12/01/16
Version 14
10/19/16: MPCTAC
11/09/16: QIC
12/01/16
Industry-wide change to applicable code
description (HCPCS code E0740) effective
01/01/17.
01/01/17
Version 15
Not applicable
because industry-wide
change in code
description.
10/01/17
Review for effective date 01/01/18. Revised
criteria in the Medical Policy Statement and
Limitations sections (designating service
experimental and investigational for the
treatment of urinary incontinence and/or fecal
incontinence). Administrative changes made to
the Policy Summary, Description of Item or
Service, Definitions, Clinical Background
Information, References, and Other Applicable
Policies sections. Plan notes updated in the
Applicable Coding section and revised code list;
diagnosis codes added for fecal incontinence
and applicable procedure codes considered
experimental and investigational for specified
indications.
01/01/18
Version 16
10/18/17: MPCTAC
10/01/18
Review for effective date 11/01/18.
Administrative changes made to the Policy
Summary, References, and Other Applicable
Policies sections. Administrative change made
to the Applicable Coding section (using ICD-10
diagnosis code range rather than individual
diagnosis codes without changing the code list).
11/01/18
Version 17
10/17/18: MPCTAC
12/01/18
Review for effective date 03/01/19. Revised the
policy title. Administrative changes made to the
Policy Summary, Description of Item or Service,
Definitions, and References sections. Criteria
updated in the Medical Policy Statement and
Limitations sections. Revised the diagnosis
codes and Plan notes in the Applicable Coding
section.
03/01/19
Version 18
12/19/18: MPCTAC
07/01/19
Review for effective date 08/01/19. Updated
the Plan notes in the Applicable Coding section.
08/01/19
Version 19
07/17/19: MPCTAC
Pelvic Floor Stimulation for the Treatment of Incontinence and/or Overactive Bladder
14 of 14
09/01/19
Review for effective date 10/01/19.
Administrative changes made to the Other
Applicable Policies, References, and Reference
to Applicable Laws and Regulations sections.
10/01/19
Version 20
09/18/19: MPCTAC
09/01/20
Review for effective date 10/01/20.
Administrative changes made to the References
and Other Applicable Policies sections.
10/01/20
Version 21
09/16/20: MPCTAC
05/01/21
Review for effective date 06/01/21. Plan note
revised in the Applicable Coding section.
Administrative changes made to the Policy
Summary, Description of Item or Service,
Medical Policy Statement, and Limitations
sections.
06/01/21
Version 22
05/19/21: MPCTAC
10/01/21
Review for effective date 11/01/21. Adopted new
medical policy template; removed administrative
sections and the Medical Policy Statement
section renamed the Clinical Criteria section.
Added NH Medicare Advantage HMO as an
applicable product effective 01/01/22.
Administrative changes made to the Policy
Summary, Clinical Criteria, Applicable Coding,
and References sections. Removed the
Limitations section.
11/01/21
Version 23
10/20/21: MPCTAC
08/01/22
Review for effective date 09/01/22.
Administrative changes made to the Clinical
Criteria and References sections.
09/01/22
Version 24
08/26/22: MPCTAC
(electronic vote)
08/01/22
Review for policy retired date 11/01/22.
Administrative changes made to the Policy
Summary and Applicable Coding sections.
Medical policy criteria revised in the Clinical
Criteria and Limitations and Exclusions sections.
Service will be managed by AIM Specialty Health
as of 11/01/22 with AIM prior authorization
required.
11/01/22
Version 25
Version 25 NOT
implemented;
Version 24 effective
09/01/22 to
11/30/22
08/26/22: MPCTAC
(electronic vote)
09/01/22
Review for policy retired date 12/01/22. The
effective date of AIM Specialty Health’s
management this service changed from 11/01/22
to 12/01/22. Administrative changes made to
the Policy Summary and Applicable Coding
sections. Medical policy criteria revised in the
Clinical Criteria and Limitations and Exclusions
sections.
12/01/22
Version 26
09/23/22: MPCTAC
(electronic vote)
Physical Therapy in the Outpatient Setting (NH Products)
1 of 12
Medical Policy – Policy with InterQual Criteria Retired and AIM Criteria Adopted as of 12/01/22
Physical Therapy in the Outpatient Setting
Policy Number: OCA 3.544
Version Number: 26
Policy Retired Date: 12/01/22
Impacted Products
☐ All Products
☒ NH Medicaid
☒ NH Medicare Advantage
☐ MA MassHealth ACO
☐ MA MassHealth MCO
☐ MA Qualified Health Plans/Employer Choice Direct
☐ MA Senior Care Options
Note: Disclaimer and audit information is located at the end of this document.
Policy Summary
The Plan considers outpatient physical therapy (PT) medically necessary, including habilitative services
and/or rehabilitative services, when AIM clinical appropriateness guidelines are met for an adult or
pediatric member or are required EPSDT services for a member age 20 or younger on the date of
service. Prior authorization from AIM Specialty Health is required for outpatient PT after the initial
evaluation. PT must be provided within the scope of practice of the treating professional and/or
paraprofessional and follow all applicable state licensing and supervisory requirements.
Clinical Criteria
No medical policy criteria.
Limitations and Exclusions
None.
Variations
The Plan uses guidance from the Centers for Medicare & Medicaid Services (CMS) for medical
necessity and coverage determinations for NH Medicare Advantage members, including but not
limited to national coverage determinations (NCDs), local coverage determinations (LCDs), local
coverage articles (LCAs), and documentation included in Medicare manuals. At the time of the Plan’s
Physical Therapy in the Outpatient Setting (NH Products)
2 of 12
most recent policy review, no applicable clinical guidelines were found from CMS. Verify CMS criteria
in effect for the requested service on the date of the prior authorization request for a SCO or NH
Medicare Advantage HMO member. When there is no guidance from CMS for the requested service
for the specified indication on the date of the prior authorization request, Plan-adopted clinical review
criteria will be used to determine the medical necessity of the service.
Applicable Coding
The Plan utilizes up-to-date, industry-standard Current Procedural Terminology (CPT) codes, Health
Care Common Procedure Coding System (HCPCS) codes, and International Statistical Classification
of Diseases and Related Health Problems, 10th revision (ICD-10) diagnosis codes in the Plan’s medical
policies. The list of applicable codes included in this policy is informational only and may not be all
inclusive. Applicable codes are subject to change without prior notification and do not guarantee
member coverage or provider reimbursement. Review the Plan’s reimbursement policies for Plan
billing guidelines. Providers are responsible for obtaining prior authorization from AIM for physical
therapy, even if an applicable code appropriately describing the service is not included in this policy’s
Applicable Coding section. Providers are expected to report all services using the most up-to-date,
industry-standard procedures and diagnosis codes at the time of the service.
CPT Codes
Code Descriptions
97010
Application of a modality to 1 or more areas; hot or cold packs
97012
Application of a modality to 1 or more areas; traction, mechanical
97014
Application of a modality to 1 or more areas; electrical stimulation (unattended)
97016
Application of a modality to 1 or more areas; vasopneumatic devices
97018
Application of a modality to 1 or more areas; paraffin bath
97022
Application of a modality to 1 or more areas; whirlpool
97024
Application of a modality to 1 or more areas; diathermy (e.g., microwave)
97026
Application of a modality to 1 or more areas; infrared
97028
Application of a modality to 1 or more areas; ultraviolet
97032
Application of a modality to 1 or more areas; electrical stimulation (manual), each 15 minutes
97033
Application of a modality to 1 or more areas; iontophoresis, each 15 minutes
97034
Application of a modality to 1 or more areas; contrast baths, each 15 minutes
97035
Application of a modality to 1 or more areas; ultrasound, each 15 minutes
97036
Application of a modality to 1 or more areas; Hubbard tank, each 15 minutes
97110
Therapeutic procedure, 1 or more areas, each 15 minutes; therapeutic exercises to develop
strength and endurance, range of motion and flexibility
97112
Therapeutic procedure, 1 or more areas, each 15 minutes; neuromuscular reeducation of
movement, balance, coordination, kinesthetic sense, posture, and/or proprioception for
sitting and/or standing activities
97113
Therapeutic procedure, 1 or more areas, each 15 minutes; aquatic therapy with therapeutic
exercises
97116
Therapeutic procedure, 1 or more areas, each 15 minutes; gait training (includes stair
climbing)
Physical Therapy in the Outpatient Setting (NH Products)
3 of 12
97124
Therapeutic procedure, 1 or more areas, each 15 minutes; massage, including effleurage,
petrissage and/or tapotement (stroking, compression, percussion)
97129
Therapeutic interventions that focus on cognitive function (e.g., attention, memory,
reasoning, executive function, problem solving, and/or pragmatic functioning) and
compensatory strategies to manage the performance of an activity (e.g., managing time or
schedules, initiating, organizing, and sequencing tasks), direct (one-on-one) patient
contact; initial 15 minutes
97130
Therapeutic interventions that focus on cognitive function (e.g., attention, memory,
reasoning, executive function, problem solving, and/or pragmatic functioning) and
compensatory strategies to manage the performance of an activity (e.g., managing time or
schedules, initiating, organizing, and sequencing tasks), direct (one-on-one) patient
contact; each additional 15 minutes (List separately in addition to code for primary
procedure)
97140
Manual therapy techniques (e.g., mobilization/manipulation, manual lymphatic drainage,
manual traction), 1 or more regions, each 15 minutes
97150
Therapeutic procedure(s), group (2 or more individuals)
97164
Re-evaluation of physical therapy established plan of care, requiring these components: An
examination including a review of history and use of standardized tests and measures is
required; and revised plan of care using a standardized patient assessment instrument
and/or measurable assessment of functional outcome. Typically, 20 minutes are spent
face-to-face with the patient and/or family.
97530
Therapeutic activities, direct (one-on-one) patient contact by the provider (use of dynamic
activities to improve functional performance), each 15 minutes
97533
Sensory integrative techniques to enhance sensory processing and promote adaptive
responses to environmental demands, direct (one-on-one) patient contact, each 15
minutes
97535
Self-care/home management training (e.g., activities of daily living (ADL) and
compensatory training, meal preparation, safety procedures, and instructions in use of
assistive technology devices/adaptive equipment) direct one-on-one contact, each 15
minutes
97537
Community/work reintegration training (e.g., shopping, transportation, money
management, avocational activities and/or work environment/modification analysis, work
task analysis, use of assistive technology device/adaptive equipment), direct one-on-one
contact, each 15 minutes
97545
Work hardening/conditioning; initial 2 hours
97546
Work hardening/conditioning; each additional hour (List separately in addition to code for
primary procedure)
97750
Physical performance test or measurement (e.g., musculoskeletal, functional capacity), with
written report, each 15 minutes
97755
Assistive technology assessment (e.g., to restore, augment or compensate for existing
function, optimize functional tasks and/or maximize environmental accessibility), direct
one-on-one contact, with written report, each 15 minutes
97760
Orthotic(s) management and training (including assessment and fitting when not otherwise
reported), upper extremity(ies), lower extremity(ies) and/or trunk, initial orthotic(s)
encounter, each 15 minutes

Physical Therapy in the Outpatient Setting (NH Products)
4 of 12
97761
Prosthetic training, upper and/or lower extremity(ies), initial prosthetic(s) encounter, each
15 minutes
97763
Orthotic(s)/prosthetic(s) management and/or training, upper extremity(ies), lower
extremity(ies), and/or trunk, subsequent orthotic(s)/prosthetic(s) encounter, each 15
minutes
References
American Association of Acupuncture and Oriental Medicine (AAAOM). AAAOM Position Statement
on Trigger Point Dry Needling (TPDN) and Intramuscular Manual Therapy (IMT).
American College of Physicians (ACP), American Pain Society (APS). Chou R, Qaseem A, Snow V,
Casey D, Cross JT Jr, Shekelle P, Owens DK; Clinical Efficacy Assessment Subcommittee of the ACP;
ACP; APS Low Back Pain Guidelines Panel. Diagnosis and treatment of low back pain: a joint clinical
practice guideline from the ACP and the APS. Ann Intern Med. 2007 Oct 2;147(7):478-91. Erratum
in: Ann Intern Med. 2008 Feb 5;148(3):247-8. PMID: 17909209.
American College of Physicians (ACP). Qaseem A, Wilt TJ, McLean RM, Forciea MA; Clinical Guidelines
Committee of the ACP. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A
Clinical Practice Guideline from the ACP. Ann Intern Med. 2017 Apr 4;166(7):514-30. doi: 10.7326/M16-
2367. Epub 2017 Feb 14. PMID: 28192789.
American Heart Association/American Stroke Association. Winstein CJ, Stein J, Arena R, Bates B,
Cherney LR, Cramer SC, Deruyter F, Eng JJ, Fisher B, Harvey RL, Lang CE, MacKay-Lyons M,
Ottenbacher KJ, Pugh S, Reeves MJ, Richards LG, Stiers W, Zorowitz RD; American Heart Association
Stroke Council, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and
Council on Quality of Care and Outcomes Research. Guidelines for Adult Stroke Rehabilitation and
Recovery: A Guideline for Healthcare Professionals From the American Heart Association/American
Stroke Association. Stroke. 2016 Jun;47(6):e98-e169. doi: 10.1161/STR.0000000000000098. Epub
2016 May 4. Review. Erratum in: Stroke. 2017 Feb;48(2):e78. Stroke. 2017 Dec;48(12 ):e369. PMID:
27145936.
American Pain Society (APS). Guideline Summaries.
American Physical Therapy Association (APTA). APTA Clinical Practice Guidelines Development
Manual.
American Physical Therapy Association (APTA). Balance and Falls.
American Physical Therapy Association (APTA). Clinical Practice Guidelines (CPGs) Developed by
APTA.
American Physical Therapy Association (APTA). Coding and Billing.
Physical Therapy in the Outpatient Setting (NH Products)
5 of 12
American Physical Therapy Association (APTA). Direction and Supervision of the Physical Therapist
Assistant.
American Physical Therapy Association (APTA). Dry Needling.
American Physical Therapy Association (APTA). Ethics and Professionalism. Code of Ethics for the
Physical Therapist, Standards of Ethical Conduct for the PTA, Value-Based Behaviors for the PTA,
Core Values for the PT and PTA, Standards of Practice for Physical Therapy.
American Physical Therapy Association (APTA). Guide to Physical Therapist Practice. Guide 3.0. 2016.
American Physical Therapy Association (APTA). Physical Therapy Documentation of Patient/Client
Management.
American Physical Therapy Association (APTA). Supervision and Teamwork.
American Society of Anesthesiologists (ASA), American Society of Regional Anesthesia and Pain
Medicine (ASRA). Rosenquist RW, Benzon HT, Connis RT, De Leon-Casasola OA, Glass D, Korevaar
WC, Cynwyd B, Mekhail NA, Merrill DG, NIckinovich DG, Rathnmell JP, Nai-Mei Sang C, Simon DL; ASA
Task Force on Chronic Pain Management. Practice guidelines for chronic pain management: an
updated report by the ASA Task Force on Chronic Pain Management and the ASRA. Anesthesiology.
2010 Apr;112(4):810-33. doi: 10.1097/ALN.0b013e3181c43103. PMID: 20124882.
Centers for Medicare & Medicaid Services (CMS). Early and Periodic Screening, Diagnostic and
Treatment (EPSDT). Medicaid.gov.
Centers for Medicare & Medicaid Services (CMS). EPSDT – A Guide for States: Coverage in the
Medicaid Benefit for Children and Adolescents. 2014 Jun.
Centers for Medicare and Medicaid Services (CMS). Manuals. Publication # 100-02. Medicare Benefit
Policy Manual.
Centers for Medicare and Medicaid Services (CMS). Manuals. Publication # 100-03. Medicare National
Coverage Determinations (NCD) Manual.
Centers for Medicare & Medicaid Services (CMS). National Coverage Determination (NCD)
Neuromuscular Electrical Stimulation (NMES) 160.12. Version 2. 2006 Oct 1.
Cruickshank TM, Reyes AR, Ziman MR. A systematic review and meta-analysis of strength training in
individuals with multiple sclerosis or Parkinson disease. Medicine (Baltimore). 2015 Jan;94(4):e411. doi:
10.1097/MD.0000000000000411. PMID: 25634170.

Physical Therapy in the Outpatient Setting (NH Products)
6 of 12
Hayes. Health Technology Assessment. Cognitive Rehabilitation Therapy for Traumatic Brain Injury
(TBI). Dallas, TX: Hayes; 2017 Sep 26. Annual Review 2021 Feb 8.
Madsen M, Larsen K, Madsen IK, Søe H, Hansen TB. Late group-based rehabilitation has no advantages
compared with supervised home-exercises after total knee arthroplasty. Dan Med J. 2013
Apr;60(4):A4607. PMID: 23651717.
Monticone M, Ferrante S, Rocca B, Baiardi P, Farra FD, Foti C. Effect of a long-lasting multidisciplinary
program on disability and fear-avoidance behaviors in patients with chronic low back pain: results of a
randomized controlled trial. Clin J Pain. 2013 Nov;29(11):929-38. doi: 10.1097/AJP.0b013e31827fef7e.
PMID: 23328343.
New Hampshire Department of Health and Human Services. Billing Manuals.
New Hampshire Department of Health and Human Services. NH Medicaid Program.
New Hampshire Department of Health and Human Services. Provider Notices.
New Hampshire Medicaid. Therapies. Physical, Occupational, Speech. Provider Manual. Volume II. 2017
Dec 1.
New Hampshire Office of Professional Licensure and Certification. Office of Licensed Allied Health
Professionals. Laws and Administrative Rules Governing Licensed Allied Health Professionals.
Parikh SS, Baxi N, Padavan SA. Musculoskeletal medicine. In: Sackheim KA, editor. Rehab Clinical
Pocket Guide. New York, NY: Springer; 2013:357-426.
Reid MC, Eccleston C, Pillemer K. Management of chronic pain in older adults. BMJ. 2015 Feb
13;350:h532. doi: 10.1136/bmj.h532. PMID: 25680884.
Schaufele MK, Tate JL. Lumbar degenerative disease. In: Frontera WR, Silver JK, Rizzo TD Jr, editors.
Essentials of Physical Medicine and Rehabilitation: Musculoskeletal Disorders, Pain, and Rehabilitation.
3rd ed. Philadelphia, PA: Elsevier Saunders; 2015:225-32.
Stanos SP, Tybursky MD, Harden RN. Chronic pain. In: Cifu DX, et al., editors. Braddom's Physical
Medicine and Rehabilitation. 5th ed. Elsevier; 2016:809-33.
Next Review Date
Not applicable
Physical Therapy in the Outpatient Setting (NH Products)
7 of 12
Retired Date
12/01/22
Authorizing Entity
MPCTAC
Appendix
Appendix: Policy History
Disclaimer Information:
Plan refers to Boston Medical Center Health Plan, Inc. which operates under the trade name WellSense Health Plan. Medical
Policies are the Plan’s guidelines for determining the medical necessity of certain services or supplies for purposes of
determining coverage. These Policies may also describe when a service or supply is considered experimental or
investigational, or cosmetic. In making coverage decisions, the Plan uses these guidelines and other Plan Policies, as well as
the Member’s benefit document, and when appropriate, coordinates with the Member’s health care Providers to consider the
individual Member’s health care needs.
Plan Policies are developed in accordance with applicable state and federal laws and regulations, and accrediting organization
standards (including NCQA). Medical Policies are also developed, as appropriate, with consideration of the medical necessity
definitions in various Plan products, review of current literature, consultation with practicing Providers in the Plan’s service
area who are medical experts in the particular field, and adherence to FDA and other government agency policies. Applicable
state or federal mandates, as well as the Member’s benefit document, take precedence over these guidelines. Policies are
reviewed and updated on an annual basis, or more frequently as needed. Treating providers are solely responsible for the
medical advice and treatment of Members.
The use of this Policy is neither a guarantee of payment nor a final prediction of how a specific claim(s) will be adjudicated.
Reimbursement is based on many factors, including member eligibility and benefits on the date of service; medical necessity;
utilization management guidelines (when applicable); coordination of benefits; adherence with applicable Plan policies and
procedures; clinical coding criteria; claim editing logic; and the applicable Plan – Provider agreement.
Physical Therapy in the Outpatient Setting (NH Products)
8 of 12
Appendix: Policy History
Original
Approval Date
Original Effective
Date* and Version
Policy Owner
Original Policy
Approved by
Regulatory Approval: N/A
Internal Approval:
09/16/05
09/16/05
Version 1
Director of Medical Policy as
Chair of Medical Policy,
Criteria, and Technology
Assessment Committee
(MPCTAC)
Quality and Clinical
Management
Committee
(Q&CMC)
*Effective Date for NH Medicaid Product: 01/01/13
*Effective Date for NH Medicare Advantage HMO Product: 01/01/22
Physical Therapy policy renumbered OCA 3.544 for physical therapy provided to NH Medicaid members age 21 or
older in the outpatient setting as of 01/11/15. (Policy formerly numbered OCA 3.54 for physical therapy in the
outpatient setting for all adult and pediatric NH Medicaid members from 01/01/13 to 01/10/15.) Policy title
changed to Physical Therapy in the Outpatient Setting as of 12/01/21.
Policy Revisions History
Review Date
Summary of Revisions
Revision
Effective Date
and Version
Number
Approved by
02/07/06
Added definitions for modality and visit. Defined
coverage for visits, evaluations and units billed.
Version 2
02/07/06: Q&CMC
07/06/06
Removed verbiage regarding reimbursement for
evaluation and modality services.
Version 3
07/06/06: Q&CMC
03/27/07
Policy archived.
Not applicable
Not specified
10/14/08
Reviewed policy and updated clinical criteria,
effective date of the revised policy is 12/16/08.
12/16/08
Version 4
11/10/08: MPTAC
12/16/08: Quality
Improvement
Committee (QIC)
09/22/09
No changes.
Version 5
09/22/09: MPCTAC
10/28/09: QIC
10/01/10
Updated template and references.
Version 6
10/20/10: MPCTAC
11/22/10: QIC
10/01/11
Added Commercial benefit limitations, updated
coding and references.
Version 7
10/19/11: MPCTAC
11/29/11: QIC
08/01/12
Off cycle review for WellSense New Hampshire
Medicaid product, revised Summary statement,
reformatted Medical Policy Statement, revised
Applicable Coding introductory paragraph,
Version 8
08/13/12: MPCTAC
09/06/12: QIC

Physical Therapy in the Outpatient Setting (NH Products)
9 of 12
updated code list, revised Limitations section,
and revised references.
11/01/12
Review for effective date 03/01/13. Updated
references. Revised Summary section. Clarified
text in Medical Policy Statement section.
Revised language in introductory paragraph in
Applicable Coding section and updated
applicable code list. Clinical criteria moved from
Clinical Background and Summary sections to
Medical Policy Statement section. Moved
services not considered medically necessary
from the Medical Policy Statement section to
the Limitations section. Removed duplicate text
from Clinical Background Information section.
Referenced Plan reimbursement policy 4.609
for physical therapy reimbursement guidelines.
Removed “Guideline” from title.
03/01/13
Version 9
11/21/12: MPCTAC
12/20/12: QIC
08/14/13 and
08/15/13:
Off cycle review for the NH Medicaid product
and merged policy format. Incorporate policy
revisions dated 11/01/12 (as specified above) for
the NH Medicaid product; these policy revisions
were approved by MPCTAC on 11/21/12 and QIC
on 12/20/12 for applicable Plan products.
Version 10
08/14/13: MPCTAC
(electronic vote)
08/15/13: QIC
11/01/13,
12/01/13,
01/01/14, and
02/01/14
Review for effective date 05/01/14. Updated
code definitions, introductory paragraph in
Applicable Coding section, and the applicable
code lists for the MA products and the NH
Medicaid product. Updated references.
Removed prior authorization waiver for the first
32 units of PT for the NH Medicaid product. Add
criterion in the Medical Policy Statement
sections for the MA products and NH Medicaid
product requiring an updated physician
prescription and supporting clinical
documentation after 20 OT visits per treatment
episode. Revised Limitations sections.
05/01/14
Version 11
02/11/14: MPCTAC
02/18/14: QIC
09/08/14
For NH Medicaid product only, waived prior
authorization of first eight (8) 15-minute
treatment units per member per servicing
provider per calendar year.
10/01/14
Version 11
Addendum A
09/17/14: MPCTAC
09/30/14: QIC
11/04/14 and
11/19/14
Review for effective date 01/11/15. Summary and
Medical Policy Statement sections updated with
guidelines specified in version 11, addendum A.
Policy renumbered OCA 3.544 to include
physical therapy in the outpatient setting for NH
Medicaid members age 21 or older on the date of
01/11/15
Version 12
11/06/14: MPCTAC
(electronic vote)
11/11/14: QIC
(electronic vote)
11/19/14: MPCTAC
12/10/14: QIC
Physical Therapy in the Outpatient Setting (NH Products)
10 of 12
service. Revised Limitations section. (PT
services formerly included in policy number OCA
3.54 for all adult and pediatric members.)
Revised review calendar.
11/01/15
Review for effective date 01/01/16. Updated
template, Summary section, and References
section. Administrative changes made to the
Medical Policy Statement and Limitations
section without changing criteria. Revised
language in the Applicable Coding section.
Added definitions.
01/01/16
Version 13
12/03/15: MPCTAC
(electronic vote)
12/09/15: QIC
12/01/16
Review for effective date 02/01/17. Industry-
wide revisions of applicable codes. Clarified
existing criteria in the Medical Policy Statement
section.
02/01/17
Version 14
12/21/16: MPCTAC
01/11/17: QIC
12/01/17
Review for effective 01/01/18. Industry-wide
updates to codes included in the Applicable
Coding section. Annual review of policy with
administrative changes made to the Definitions
and Reference sections.
01/01/18
Version 15
12/20/17: MPCTAC
02/01/18
Review for effective date 03/01/18.
Administrative changes made to the Policy
Summary and Limitations sections.
03/01/18
Version 16
02/21/18: MPCTAC
11/01/18
Review for effective date 12/01/18.
Administrative changes made to the Policy
Summary, Medical Policy Statement, Limitations,
Definitions, References, Other Applicable
Policies, and Reference to Applicable Laws and
Regulations sections.
12/01/18
Version 17
11/21/18: MPCTAC
03/01/19
Review for effective date 07/01/19.
Administrative changes made to the Limitations
and Reference to Applicable Laws and
Regulations sections. Criteria revised in the
Medical Policy Statement section.
07/01/19
Version 18
03/20/19: MPCTAC
12/01/19
Review for effective date 01/01/20. Industry-
wide updates to codes included in the Applicable
Coding section.
01/01/20
Version 19
Not applicable
because industry-wide
code changes
11/01/19
Review for effective date 02/01/20.
Administrative changes made to the References
and Reference to Applicable Laws and
Regulations sections. Revised criteria in the
Medical Policy Statement and Limitations
sections.
02/01/20
Version 20
Renumbered to
version 20 to
implement
industry-wide
code updates
effective 01/01/20
11/20/19: MPCTAC
Physical Therapy in the Outpatient Setting (NH Products)
11 of 12
included in version
19
12/01/19
Review for effective 02/01/20. Industry-wide
updates to codes effective 01/01/20 included in
the Applicable Coding section of the policy
version 20 effective 02/01/20.
02/01/20
Version 21
12/18/19: MPCTAC
12/01/19
Review for effective date 03/01/20. Revised in
the Medical Policy Statement section the
definition of a servicing PT provider for the prior
authorization waiver.
03/01/20
Version 22
12/18/19: MPCTAC
11/01/20
Review for effective date 12/01/20. Updated the
References section. Administrative change
made to the Applicable Coding section.
12/01/20
Version 23
11/18/20: MPCTAC
11/01/21
Review for effective date 12/01/21. Adopted new
medical policy template; removed administrative
sections, Medical Policy Statement section
renamed Clinical Criteria section, and Limitations
section renamed Limitations and Exclusions
section. Administrative changes made to the
Policy Summary, Applicable Coding, and
References sections. Medical policy criteria
retired and InterQual criteria will continue to be
used to determine the medical necessity of
services. Revised policy title because policy
applies to adult and pediatric members as of
12/01/21.
12/01/21
Version 24
11/17/21: MPCTAC
08/01/22
Review for policy retired date 11/01/22.
Administrative changes made to the Policy
Summary and Applicable Coding sections.
InterQual medical necessity criteria and medical
policy guidelines in the Clinical Criteria and
Limitations and Exclusions sections retired on
11/01/22. AIM criteria adopted for outpatient PT
on 11/01/22. Plan prior authorization waivers
removed after 10/31/22. AIM prior authorization
is required for outpatient PT after the initial
evaluation as of 11/01/22, even when applicable
codes are not listed in this Plan policy.
11/01/22
Version 25
Version 25 NOT
implemented;
Version 24
effective 12/01/21
to 11/30/22
08/26/22: MPCTAC
(electronic vote)
09/01/22
Review for policy retired date 12/01/22. The
effective date of AIM Specialty Health’s
management of outpatient rehabilitation
services changed from 11/01/22 to 12/01/22.
Administrative changes made to the Policy
Summary and Applicable Coding sections.
InterQual medical necessity criteria and medical
policy guidelines in the Clinical Criteria and
12/01/22
Version 26
09/23/22: MPCTAC
(electronic vote)
Physical Therapy in the Outpatient Setting (NH Products)
12 of 12
Limitations and Exclusions sections retired as of
12/01/22. AIM criteria adopted for outpatient PT
for dates of service on or after 12/01/22. Plan
prior authorization waivers removed after
11/30/22. AIM prior authorization is required for
outpatient PT after the initial evaluation as of
12/01/22, even when applicable codes are not
listed in this Plan policy.
Sacral Nerve Stimulation (Including Peripheral Nerve Stimulation Test and Two-Stage Tined Lead Procedure)
for Incontinence and Urinary Conditions
1 of 22
Medical Policy
Sacral Nerve Stimulation (Including Peripheral Nerve Stimulation
Test and Two-Stage Tined Lead Procedure) for Incontinence and
Urinary Conditions or Incontinence and Urinary Conditions
Policy Number: OCA 3.563
Version Number: 21
Version Effective Date: 12/01/22
Impacted Products
☒ All Products
☒ NH Medicaid
☒ NH Medicare Advantage
☒ MA MassHealth ACO
☒ MA MassHealth MCO
☒ MA Qualified Health Plans/Employer Choice Direct
☒ MA Senior Care Options
+
Note: Disclaimer and audit information is located at the end of this document.
Policy Summary
The Plan considers implantable sacral nerve stimulation (SNS), also known as sacral neuromodulation,
to be medically necessary when applicable medical criteria are met; this includes peripheral nerve
stimulation test and tined lead procedure before the implantation of the permanent SNS device. Plan
prior authorization is required.
Clinical Criteria
Sacral nerve stimulation (SNS) initial testing or permanent implantation of a SNS device (e.g.,
InterStim™ system by Medtronic, Inc.) is considered medically necessary when applicable Plan criteria
are met in EITHER item I or item II:
I. Medical Necessity Criteria:
A. Sacral Nerve Stimulation (SNS) to Treat Urinary Conditions:
Sacral Nerve Stimulation (Including Peripheral Nerve Stimulation Test and Two-Stage Tined Lead Procedure)
for Incontinence and Urinary Conditions
2 of 22
Applicable criteria must be met based on the phase of treatment in EITHER item 1 (Initial
Testing Phase) or item 2 (Permanent Implantation):
1. Initial Testing Phase for Implanted SNS:
Trial period of implantable SNS (with either peripheral nerve stimulation or a temporarily
implanted lead with stage one of the tined lead procedure) is considered medically
necessary when ALL criteria are met in items a through f:
a. Member is experiencing at least ONE (1) of the urinary symptoms in items (1) through
(3) for at least 6 months:
(1) Non-obstructive urinary retention; OR
(2) Urgency-frequency syndrome; OR
(3) Urinary urge incontinence; AND
b. Member’s urinary symptoms are NOT related to a neurologic condition; AND
c. Member’s conservative treatment meets ONE (1) of the criteria in item (1) or item (2):
(1) Member is medically refractory to conservative therapy and has failed 6 months of
behavioral therapy and 3 months of pharmacological therapy (which included a
trial of at least 2 anti-cholinergic agents or a trial of 1 anti-cholinergic agent and 1
beta 3 adrenergic receptor agonist); OR
(2) Member cannot tolerate a minimum of 6 consecutive months of conservative
treatment due to a significant disability (e.g., frequency or severity impacts ability
to work or participate in activities outside of the home); AND
d. Member is 18 years of age or older on the date of service; AND
e. Member is willing to comply with the treatment protocol and has the cognitive capacity
to use the remote control to optimize device function during the testing and treatment
phases; AND
f. Member’s current treatment plan does NOT include the use of percutaneous tibial nerve
stimulation (PTNS) for non-neurogenic urinary overactive bladder symptoms; OR
2. Permanent Implantation of SNS:
Sacral Nerve Stimulation (Including Peripheral Nerve Stimulation Test and Two-Stage Tined Lead Procedure)
for Incontinence and Urinary Conditions
3 of 22
Permanent implantation of a SNS device is considered medically necessary when BOTH
criteria are met in item a and item b:
a. Member meets all the criteria listed above for the peripheral nerve stimulation test or
stage one of the tined lead procedure (to estimate potential response to SNS); AND
b. Member has experienced a 50% or greater relief of incontinence or primary symptoms
for at least 48 hours during the percutaneous trial or stage one of the tined lead test as
measured by voiding diaries; OR
B. Sacral Nerve Stimulation (SNS) to Treat Chronic Fecal Incontinence:
Applicable criteria must be met based on the phase of treatment in EITHER item 1 (Initial
Testing Phase) or item 2 (Permanent Implantation):
1. Initial Testing Phase of Implanted SNS:
Trial period of implantable SNS (with either peripheral nerve stimulation or a temporarily
implanted lead with stage one of the tined lead procedure) is considered medically
necessary to treat fecal incontinence after review and approval of a Plan Medical Director
and when ALL criteria are met in items a through f:
a. Member has chronic fecal incontinence with greater than 2 incontinent episodes on
average per week for at least 6 months in duration or for at least 12 months after vaginal
childbirth; AND
b. Member’s fecal incontinence is NOT related to a neurologic condition; AND
c. Member’s conservative treatment (before the request for the initial testing phase of
implanted sacral nerve stimulation) meets ONE (1) of the criteria in item (1) or item (2):
(1) Member is medically refractory to conservative therapy and BOTH criteria are met
in item (a) and item (b):
(a) Failure of behavioral therapy (e.g., dietary modification, pelvic floor
retraining); AND
(b) Failure of pharmacological therapy; AND
(2) Member cannot tolerate conservative treatment due to a significant disability
(e.g., frequency or severity impacts ability to work or participate in activities
outside of the home); AND

Sacral Nerve Stimulation (Including Peripheral Nerve Stimulation Test and Two-Stage Tined Lead Procedure)
for Incontinence and Urinary Conditions
4 of 22
d. If the member has medical history of chronic inflammatory bowel disease (IBD), IBD
does NOT involve the anorectum; AND
e. Member is 18 years of age or older on the date of service; AND
f. Member is willing to comply with the treatment protocol and has the cognitive capacity
to use the remote control to optimize device function during the testing and treatment
phases; OR
C. Permanent Implantation of SNS:
1. Permanent implantation of a SNS device for the treatment of fecal incontinence is
considered medically necessary after review and approval of a Plan Medical Director and
when ALL criteria are met in items a and b:
a. Member meets all the criteria above for the peripheral nerve stimulation test or stage
one of the tined lead procedure (to estimate potential response to SNS); AND
b. Member has experienced a 50% or greater relief of incontinence symptoms for at least
48 hours during the percutaneous trial or stage one of the tined lead test as measured
by elimination journals.
II. Plan Medical Director review is required for any of the following requests:
A. The use of an implantable sacral nerve stimulation (SNS) for members age 16 or 17 on the date
of service; OR
B. All requests for implantable SNS (including initial testing phase and/or permanent
implantation) to treat fecal incontinence; in addition, ALL applicable criteria in item IB above
(Sacral Nerve Stimulation to Treat Chronic Fecal Incontinence) must be met and documented
in the member’s medical record.
Limitations and Exclusions
A. Contraindications for the use of implantable SNS (including associated testing) include any of
the following conditions for the member:
1. Chronic inflammatory bowel disease involving the anorectum mechanical obstruction, or
malformation in the applicable anatomical area; OR
2. Receiving any form of diathermy or is expected to receive diathermy during the duration of
treatment with sacral nerve stimulation; OR
3. Member has a pacemaker or implantable defibrillator; OR
Sacral Nerve Stimulation (Including Peripheral Nerve Stimulation Test and Two-Stage Tined Lead Procedure)
for Incontinence and Urinary Conditions
5 of 22
4. Pregnant or plans to become pregnant during the duration of treatment with sacral nerve
stimulation; OR
5. History of rectal surgery in the previous 12 months, or in the case of cancer, the member has
had rectal surgery in the past 24 months.
B. The Plan considers ANY uses of SNS (including associated testing) listed in items 1 through 3 to
be experimental and investigational or NOT medically necessary due to limited evidence
demonstrating the clinical utility and clinical validity of SNS for these indications or conditions:
1. Member is unwilling or unable to comply with the treatment protocol and/or does not have
the cognitive capacity to use the remote control to optimize device function during the
testing and treatment phases; OR
2. The use of a wireless sacral nerve stimulator (e.g., StimGuard) because the safety and
efficacy of the wireless devices have not been adequately studied; OR
3. The use of implantable SNS (including associated testing) is considered experimental and
investigational when used for a member age 15 or younger on the date of service.
The use of posterior tibial nerve stimulation, including percutaneous tibial nerve stimulation
(PTNS) and/or transcutaneous posterior tibial nerve stimulation (TPTNS) with a member who
has an implantable SNS device or has initiated the initial testing phase of an implantable SNS.
Posterior tibial nerve stimulation may NOT be administered concurrently with SNS. Review the
Plan’s Posterior Tibial Nerve Stimulation (Percutaneous or Transcutaneous) medical policy,
policy number OCA 3.562 for applicable medical necessity criteria for these services.
Variations
The Plan uses guidance from the Centers for Medicare & Medicaid Services (CMS) for medical
necessity and coverage determinations for Senior Care Options (SCO) members and New Hampshire
Medicare Advantage HMO members, including but not limited to national coverage determinations
(NCDs), local coverage determinations (LCDs), local coverage articles (LCAs), and documentation
included in Medicare manuals. At the time of the Plan’s most recent policy review, NCD 23.18 includes
medical necessity criteria for the use of sacral nerve stimulation (SNS) for the treatment of urinary
urge incontinence, urgency-frequency syndrome, and urinary retention. Verify CMS guidelines in
effect on the date of the prior authorization request. When there is no guidance from CMS for the
requested service, Plan-adopted clinical review criteria will be used to determine the medical necessity
of the service.
Applicable Coding
The Plan utilizes up-to-date, industry-standard Current Procedural Terminology (CPT) codes, Health
Care Common Procedure Coding System (HCPCS) codes, and International Statistical Classification
Sacral Nerve Stimulation (Including Peripheral Nerve Stimulation Test and Two-Stage Tined Lead Procedure)
for Incontinence and Urinary Conditions
6 of 22
of Diseases and Related Health Problems, 10th revision (ICD-10) diagnosis codes in the Plan’s medical
policies. Since these codes may be updated at different intervals than the medical policy review cycle,
the list of applicable codes included in a policy is informational only and may not be all
inclusive. Applicable codes are subject to change without prior notification and do not guarantee
member coverage or provider reimbursement. Review the Plan’s reimbursement policies for Plan
billing guidelines. Providers are responsible for obtaining prior authorization for the services specified
in the Clinical Criteria section and Limitations and Exclusions section of a medical policy, even if an
applicable code appropriately describing the service is not included in the policy’s Applicable Coding
section. Providers are expected to report all services using the most up-to-date, industry-standard
procedures and diagnosis codes at the time of the service.
CPT Codes
Description: Codes covered when medically necessary
64561
Percutaneous implantation of neurostimulator electrode array; sacral nerve
(transforaminal placement) including image guidance, if performed
Plan note: Percutaneous trial/temporary stimulation to estimate potential response to
SNS.
64581
Open implantation of neurostimulator electrode array; sacral nerve (transforaminal
placement)
64585
Revision or removal of peripheral neurostimulator electrode array
64590
Insertion or replacement of peripheral or gastric neurostimulator pulse generator or
receiver, direct or inductive coupling
64595
Revision or removal of peripheral or gastric neurostimulator pulse generator or receiver
HCPCS Codes
Description: Codes covered when medically necessary
A4290
Sacral nerve stimulation test lead, each
E0745
Neuromuscular stimulator, electronic shock unit
L8680
Implantable neurostimulator electrode, each
Plan note: Code is NOT payable for the Senior Care Options and WellSense Medicare
Advantage HMO products.
L8681
Patient programmer (external) for use with implantable programmable neurostimulator
pulse generator, replacement only
L8682
Implantable neurostimulator radiofrequency receiver
L8683
Radiofrequency transmitter (external) for use with implantable neurostimulator
radiofrequency receiver
L8684
Radiofrequency transmitter (external) for use with implantable sacral root neurostimulator
receiver for bowel and bladder management, replacement
L8685
Implantable neurostimulator pulse generator, single array, rechargeable, includes
extension
Plan note: Code is NOT payable for the Senior Care Options and WellSense Medicare
Advantage HMO products.
L8686
Implantable neurostimulator pulse generator, single array, nonrechargeable, includes
extension
Sacral Nerve Stimulation (Including Peripheral Nerve Stimulation Test and Two-Stage Tined Lead Procedure)
for Incontinence and Urinary Conditions
7 of 22
Plan note: Code is NOT payable for the Senior Care Options and WellSense Medicare
Advantage HMO products.
L8687
Implantable neurostimulator pulse generator, dual array, rechargeable, includes extension
Plan note: Code is NOT payable for the Senior Care Options and WellSense Medicare
Advantage HMO products.
L8688
Implantable neurostimulator pulse generator, dual array, nonrechargeable, includes
extension
Plan note: Code is NOT payable for the Senior Care Options and WellSense Medicare
Advantage HMO products.
L8689
External recharging system for battery (internal) for use with implantable neurostimulator,
replacement only
L8695
External recharging system for battery (external) for use with implantable
neurostimulator, replacement only
ICD-10
Diagnosis
Codes
Description: One (1) of the following ICD-10 diagnosis c odes is required when
billing with a CPT code or HCPCS code for SNS
N32.81
Overactive bladder
N32.9
Bladder disorder, unspecified
N39.3
Stress incontinence (female)(male)
N39.41-N39.43
Other specified urinary incontinence
N39.45-N39.46
Other specified urinary incontinence
N39.490
Other specified urinary incontinence; overflow incontinence
N39.498
Other specified urinary incontinence (reflex incontinence) (total incontinence)
R15.0-R15.9
Fecal incontinence
R32
Unspecified urinary incontinence
R33.0-R33.9
Retention of urine
R35.0
Frequency of micturition
R39.14
Feeling of incomplete bladder emptying
R39.15
Urgency of urination
References
Abrams P, Andersson KE, Birder L, Brubaker L, Cardozo L, Chapple C, Cottenden A, Davila W, de
Ridder D, Dmochowski R, Drake M, Dubeau C, Fry C, Hanno P, Smith JH, Herschorn S, Hosker
G, Kelleher C, Koelbl H, Khoury S, Madoff R, Milsom I, Moore K, Newman D, Nitti V, Norton C, Nygaard
I, Payne C, Smith A, Staskin D, Tekgul S, Thuroff J, Tubaro A, Vodusek D, Wein A, Wyndaele
JJ; Members of Committees; Fourth International Consultation on Incontinence. Fourth international
consultation on incontinence recommendations of the International Scientific Committee: Evaluation
and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol
Urodyn. 2010;29(1):213-40. doi: 10.1002/nau.20870. PMID: 20025020.

Sacral Nerve Stimulation (Including Peripheral Nerve Stimulation Test and Two-Stage Tined Lead Procedure)
for Incontinence and Urinary Conditions
8 of 22
Altomare DF, Giuratrabocchetta S, Knowles CH, Muñoz Duyos A, Robert-Yap J, Matzel KE; European
SNS Outcome Study Group. Long-term outcomes of sacral nerve stimulation for fecal incontinence. Br
J Surg. 2015 Mar;102(4):407-15. doi: 10.1002/bjs.9740. Epub 2015 Feb 2. PMID: 25644687.
American College of Gastroenterology (ACG). Guidelines.
American College of Gastroenterology (ACG). Rao SS, ACG Practice Parameters Committee.
Diagnosis and management of fecal incontinence. Am J Gastroenterol. 2004 Aug;99(8):1585-604. doi:
10.1111/j.1572-0241.2004.40105.x. PMID: 15307881.
The American College of Obstetricians and Gynecologists (ACOG). Clinical Guidance.
The American College of Obstetricians and Gynecologists (ACOG). ACOG Practice Bulletin No. 155.
Urinary Incontinence in Women. Obstet Gynecol. 2015 Nov;126(5):e66-81. doi:
10.1097/AOG.0000000000001148. PMID: 26488524.
The American College of Obstetricians and Gynecologists (ACOG). ACOG Practice Bulletin No. 210.
Fecal Incontinence. Obstet Gynecol. 2019 Apr;133(4):837-9. doi: 10.1097/AOG.0000000000003188.
PMID: 30913191.
The American College of Obstetricians and Gynecologists (ACOG), American Urogynecologic Society
(AUGS). ACOG Committee on Gynecologic Practice. Evaluation of Uncomplicated Stress Urinary
Incontinence in Women Before Surgical Treatment. Committee Opinion Number 603. 2014 Jun.
Reaffirmed 2017.
The American College of Obstetricians and Gynecologists (ACOG). Urinary Incontinence. Patient
Resources.
American College of Physicians (ACP). Clinical Guidelines & Recommendations.
American College of Physicians (ACP). Qaseem A, Dallas P, Forciea MA, Starkey M, Denberg TD,
Shekelle P. Clinical Guidelines Committee of the ACP. Nonsurgical management of urinary
incontinence in women: a clinical practice guideline from the ACP. Ann Intern Med. 2014 Sep
16;161(6):429-40. doi: 10.7326/M13-2410. PMID: 25222388.
American Gastroenterological Association (AGA). Bharucha AE, Pemberton JH, Locke GR. American
Gastroenterological Association technical review on constipation. Gastroenterology. 2013
Jan;144(1):218-38. doi: 10.1053/j.gastro.2012.10.028. PMID: 23261065.
American Gastroenterological Association (AGA). Clinical Guidelines.
The American Society of Colon and Rectal Surgeons (ASCRS). Clinical Practice Guidelines.

Sacral Nerve Stimulation (Including Peripheral Nerve Stimulation Test and Two-Stage Tined Lead Procedure)
for Incontinence and Urinary Conditions
9 of 22
The American Society of Colon and Rectal Surgeons (ASCRS). Paquette IM, Varma MG, Kaiser AM,
Steele SR, Rafferty JF. The American Society of Colon and Rectal Surgeons’ clinical practice guideline
for the treatment of fecal incontinence. Dis Colon Rectum. 2015 Jul;58(7):623-36. doi:
10.1097/DCR.0000000000000397. PMID: 26200676.
American Urogynecologic Society (AUGS). Clinical Guidance Documents.
American Urological Association (AUA). Guidelines & Policies.
American Urological Association (AUA) and Society of Urodynamics, Female Pelvic Medicine &
Urogenital Reconstruction (SUFU). Lightner DJ, Gomelsky A, Souter L, Vasavada SP. Diagnosis and
Treatment of Overactive Bladder (Non-Neurogenic) in Adults: AUA/SUFU Guideline Amendment
2019. J Urol. 2019 Sep;202(3):558-63. doi: 10.1097/JU.0000000000000309. Epub 2019 Aug 8.
PMID: 31039103.
American Urological Association (AUA) and Society of Urodynamics, Female Pelvic Medicine &
Urogenital Reconstruction (SUFU). Kobashi KC, Albo ME, Dmochowski RR, Ginsberg DA, Goldman HB,
Gomelsky A, Kraus SR, Sandhu JS, Shepler T, Treadwell JR. Vasavada S, Lemack GE. Surgical
Treatment of Female Stress Urinary Incontinence (SUI): AUA/SUFU Guideline. J Urol. 2017
Oct;198(4):875-883. doi: 10.1016/j.juro.2017.06.061. Epub 2017 Jun 15. PMID: 28625508.
Amundsen CL, Richter HE, Menefee SA, Komesu YM, Arya LA, Gregory WT, Myers DL, Zyczynski HM,
Vasavada S, Nolen TL, Wallace D, Meikle SF. OnabotulinumtoxinA vs Sacral Neuromodulation on
Refractory Urgency Urinary Incontinence in Women: A Randomized Clinical Trial. JAMA. 2016 Oct
4;316(13):1366-1374. doi: 10.1001/jama.2016.14617. PMID: 27701661.
Angioli R, Montera R, Plotti F, Aloisi A, Montone E, Zullo MA. Success rates, quality of life, and feasibility
of sacral nerve stimulation in elderly patients: 1-year follow-up. Int Urogynecol J. 2013 May;24(5):789-
94. doi: 10.1007/s00192-012-1928-3. Epub 2012 Sep 8. PMID: 22961496.
Banakhar M, Hassouna M. Percutaneous Nerve Evaluation Test Versus Staged Test Trials for Sacral
Neuromodulation: Sensitivity, Specificity, and Predictive Values of Each Technique. Int Neurourol J.
2016 Sep;20(3):250–254. doi: 10.5213/inj.1630498.249. PMID: 27706006.
Barnett G, Ockrim J. Re: Cost of neuromodulation therapies for overactive bladder: percutaneous tibial
nerve stimulation versus sacral nerve stimulation: M. Martinson, S. MacDiarmid and E. Black J Urol
2013;189:210-6. J Urol. 2013 Oct;190(4):1444-5. doi: 10.1016/j.juro.2013.04.131. Epub 2013 Jul 22. PMID:
23886880.
Brégeon J, Neunlist M, Bossard C, Biraud C, Mandy B, Coron E, Bourreille A, Meurette,G. Improvement
of Refractory Ulcerative Proctitis With Sacral Nerve Stimulation. J Clin Gastroenterol. 2015
Nov/Dec;49(10):853-7. doi: 10.1097/MCG.0000000000000331. PMID: 25930972.
Sacral Nerve Stimulation (Including Peripheral Nerve Stimulation Test and Two-Stage Tined Lead Procedure)
for Incontinence and Urinary Conditions
10 of 22
Bielefeldt K. Adverse events of sacral neuromodulation for fecal incontinence reported to the federal
drug administration. World J Gastrointest Pharmacol Ther. 2016 May 6;7(2):294–305.
doi: 10.4292/wjgpt.v7.i2.294. PMID: 27158546.
Bragg R, Hebel D, Vouri SM, Pitlick JM. Mirabegron: a Beta-3 agonist for overactive bladder. Consult
Pharm. 2014 Dec;29(12):823-37. doi: 10.4140/TCP.n.2014.823. PMID: 25521658.
Canadian Urological Association. Bettez M, Tu LM, Carlson K, Corcos J, Gajewski J, Jolivet M, Bailly G.
2012 Update: Guidelines for Adult Urinary Incontinence Collaborative Consensus Document for the
Canadian Urological Association. Can Urol Assoc J. 2012 Oct;6(5):354–63. doi: 10.5489/cuaj.12248.
PMID: 23093627.
Carrington EV, Evers J, Grossi U, Dinning PG, Scott SM, O'Connell PR, Jones JF, Knowles CH. A
systematic review of sacral nerve stimulation mechanisms in the treatment of fecal incontinence and
constipation. Neurogastroenterol Motil. 2014 Sep;26(9):1222-37. doi: 10.1111/nmo.12388. PMID:
25167953.
Centers of Disease Control and Prevention (CDC). Inflammatory bowel disease (IBD). 2017 Mar 14.
Centers for Medicare & Medicaid Services (CMS). Local Coverage Determination (LCD) Posterior
Tibial Nerve Stimulation for Voiding Dysfunction L33396. National Government Services, Inc. 2015 Oct
1. Revision Effective Date 2019 Oct 24.
Centers for Medicare & Medicaid Services (CMS). Manuals. Publication # 100-02. Medicare Benefit
Policy Manual.
Centers for Medicare & Medicaid Services (CMS). Manuals. Publication # 100-03. Medicare National
Coverage Determinations (NCD) Manual.
Centers for Medicare & Medicaid Services (CMS). Medicare Coverage Database (MCD).
Centers for Medicare & Medicaid Services (CMS). National Coverage Determination (NCD) for
Bladder Stimulators (Pacemakers) 230.16. 1996 Oct 7.
Centers for Medicare & Medicaid Services (CMS). National Coverage Determination (NCD) for
Incontinence Control Devices 230.10. 1996 Oct 7.
Centers for Medicare & Medicaid Services (CMS). National Coverage Determination (NCD) for Non-
Implantable Pelvic Floor Electrical Stimulator 230.8. Effective 2006 Jun 19.
Centers for Medicare & Medicaid Services (CMS). National Coverage Determination (NCD) for Sacral
Nerve Stimulation for Urinary Incontinence 230.18. Effective 2002 Jan 1.
Centers for Medicare & Medicaid Services (CMS). Transmittals.
Sacral Nerve Stimulation (Including Peripheral Nerve Stimulation Test and Two-Stage Tined Lead Procedure)
for Incontinence and Urinary Conditions
11 of 22
Chiarioni G, Palsson OS, Asteria CR, Whitehead WE. Neuromodulation for fecal incontinence: An
effective surgical intervention. World J Gastroenterol. 2013 Nov 7;19(41):7048–54. doi:
10.3748/wjg.v19.i41.7048. PMID: 24222947.
Commonwealth of Massachusetts. Division of Insurance (DOI) Bulletins.
Commonwealth of Massachusetts. MassHealth Provider Bulletins.
Commonwealth of Massachusetts. MassHealth Provider Manuals.
Commonwealth of Massachusetts. MassHealth Transmittal Letters.
Dinning PG, Hunt L, Patton V, Zhang T, Szczesniak M, Gebski V, Jones M, Stewart P, Lubowski DZ,
Cook IJ. Treatment efficacy of sacral nerve stimulation in slow transit constipation: a two-phase,
double-blind randomized controlled crossover study. Am J Gastroenterol. 2015 May;110(5):733-40. doi:
10.1038/ajg.2015.101. Epub 2015 Apr 21. PMID: 25895520.
El-Gazzaz G, Zutshi M, Salcedo L, Hammel J, Rackley R, Hull T. Sacral neuromodulation for the
treatment of fecal incontinence and urinary incontinence in female patients: long-term follow-up. Int J
Colorectal Dis. 2009 Dec;24(12):1377-81. doi: 10.1007/s00384-009-0745-8. Epub 2009 Jun 2. PMID:
19488765.
European Association of Urology (EAU). Blok B, Castro-Diaz D, Del Popolo G, Groen J, Hamid R,
Karsenty G, Kessler TM, Pannek J, Ecclestone H, Musco S, Padilla-Fernández B, Sartori A, 't Hoen LA.
EAU Guidelines. Neuro-Urology. 2020 Mar. Edn. presented at the EAU Annual Congress Amsterdam
2022. ISBN 978-94-92671-16-5.
European Association of Urology (EAU). Gacci M, Sakalis VI, Karavitakis M, Cornu JN, Gratzke C,
Hermann TRW, Kyriazis I, Malde S, Mamoulakis C, Rieken M, Schouten N, Smith EJ, Speakman MJ,
Tikkinen KAO, Gravas S. EAU Guidelines on Male Urinary Incontinence. Rev Incon. 2022 Oct
1;82(4):387-98. doi: 10.1016/j.euro.2022.05.0122.
European Association of Urology (EAU). Nambiar AK, Arlandis S, Bo K, Cobussen-Boekhorst H,
Costantini E, de Heide M, Farag F, Groen J, Karavitakis M, Lapitan MC, Manso M, Monagas Arteaga S,
Nic An Riogh A, O’Connor E, Omar MI, Peyronnet B, Phe V, Sakalis VI, Sihra N, Tzelves L, van
Poelgeest-Pomfret ML, van den Bos TWL, van der Vaart H, Harding CK. EAU Guidelines on the
Diagnosis and Management of Female Non-Neurogenic Lower Urinary Tract Symptoms. Part 1:
Diagnostics, Overactive Bladder, Stress Urinary Incontinence, and Mixed Urinary Incontinence.
European Urology. 2022 Jul;82(1):60-70. doi: 10.1016/j.eururo.2022.01.045.
European Association of Urology (EAU). Nambiar AK, Bosch R, Cruz F, Lemack GE, Thiruchelvam N,
Tubaro A, Bedretdinova DA, Ambühl D, Farag F, Lombardo R, Schneider MP, Burkhard FC. EAU

Sacral Nerve Stimulation (Including Peripheral Nerve Stimulation Test and Two-Stage Tined Lead Procedure)
for Incontinence and Urinary Conditions
12 of 22
Guidelines on Assessment and Nonsurgical Management of Urinary Incontinence. Eur Urol. 2018
Apr;73(4):596-609. doi: 10.1016/j.eururo.2017.12.031. Epub 2018 Feb 3. PMID: 29398262.
European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN), North
American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN). Tabbers
MM, DiLorenzo C, Berger MY, Faure BC, Langendam MW, Nurko S, Staiano A, Vandenplas Y, Benninga
MA. Clinical Guideline. Evaluation and Treatment of Functional Constipation in Infants and Children:
Evidence-Based Recommendations from ESPGHAN and NASPGHAN. JPGN. 2014 Feb;58(2):258-74.
doi: 10.1097/MPG.0000000000000266.
Fritel X, Fauconnier A, Bader G, Cosson M, Debodinance P, Deffieux X, Denys P, Dompeyre P, Faltin
D, Fatton B, Haab F, Hermieux JF, Kerdraon J, Mares P, Mellier G, Michel-Laaengh N, Nadeau
C, Robain G, de Tayrac R, Jacquetin B; French College of Gynecologists and Obstetricians. Diagnosis
and management of adult female stress urinary incontinence: guidelines for clinical practice from the
French College of Gynecologists and Obstetricians. Eur J Obstet Gynecol Reprod Biol. 2010
Jul;151(1):14-9. doi: 10.1016/j.ejogrb.2010.02.041. Epub 2010 Mar 16. PMID: 20236751.
George AT, Kalmar K, Panerese A, Dudding TC, Nicholls RJ, Vaizey CJ. Long-term outcomes of sacral
nerve stimulation for fecal incontinence. Dis Colon Rectum. 2012 Mar;55(3):302-6. doi:
10.1097/DCR.0b013e3182401ecd. PMID: 22469797.
Gorissen KJ, Bloemendaal AL, Prapasrivorakul S, Gosselink MP, Jones OM, Cunningham C, Lindsey I,
Hompes R. Dynamic Article: Permanent Sacral Nerve Stimulation Under Local Anesthesia: Feasibility,
Best Practice, and Patient Satisfaction. Dis Colon Rectum. 2015 Dec;58(12):1182-5. doi:
10.1097/DCR.0000000000000489. PMID: 26544816.
Groen J, Blok BF, Bosch JL. Sacral neuromodulation as treatment for refractory idiopathic urge urinary
incontinence: 5-year results of a longitudinal study in 60 women. J Urol. 2011 Sep;186(3):954-9. doi:
10.1016/j.juro.2011.04.059. Epub 2011 Jul 24. PMID: 21791355.
Hayes. Clinical Assessment. Sacral Nerve Stimulation for Treatment of Non-obstructive Urinary
Retention. Dallas, TX: Hayes; 2022 Feb 11.
Hayes. Evolving Evidence Review. Axonics Sacral Neuromodulation (Axonics Inc ) for the Management
of Urinary Dysfunction. Dallas, TX: Hayes; 2021 Sep 1.
Hotouras A, Murphy J, Allison M, Curry A, Williams NS, Knowles CH, Chan CL. Prospective clinical audit
of two neuromodulatory treatments for fecal incontinence: sacral nerve stimulation (SNS) and
percutaneous tibial nerve stimulation (PTNS). Surg Today. 2014 Nov;44(11):2124-30. doi:
10.1007/s00595-014-0898-0. Epub 2014 May 5. PMID: 24792064.
Hotouras A, Murphy J, Thin NN, Allison M, Horrocks E, Williams NS, Knowles CH, Chan CL. Outcome of
sacral nerve stimulation for fecal incontinence in patients refractory to percutaneous tibial nerve

Sacral Nerve Stimulation (Including Peripheral Nerve Stimulation Test and Two-Stage Tined Lead Procedure)
for Incontinence and Urinary Conditions
13 of 22
stimulation. Dis Colon Rectum. 2013 Jul;56(7):915-20. doi: 10.1097/DCR.0b013e31827f0697. PMID:
23739200.
Hull T, Giese C, Wexner SD, Mellgren A, Devroede G, Madoff RD, Stromberg K, Coller JA; SNS Study
Group. Long-term durability of sacral nerve stimulation therapy for chronic fecal incontinence. Dis
Colon Rectum. 2013 Feb;56(2):234-45. doi: 10.1097/DCR.0b013e318276b24c. PMID: 23303153.
Jelovsek JE, Reddy J. Surgical management of stress urinary incontinence in women: Choosing a
primary surgical procedure. UpToDate. 2020 Apr 13. Updated: 2022 Apr 07.
Johnson BL 3rd, Abodeely A, Ferguson MA, Davis BR, Rafferty JF, Paquette IM. Is sacral
neuromodulation here to stay? Clinical outcomes of a new treatment for fecal incontinence. J
Gastrointest Surg. 2015 Jan;19(1):15-9; discussion 19-20. doi: 10.1007/s11605-014-2611-4. Epub 2014
Aug 13. PMID: 25115325.
Knowles CH, Thin N, Gill K, Bhan C, Grimmer K, Lunniss PJ, Williams NS, Scott SM. Prospective
randomized double-blind study of temporary sacral nerve stimulation in patients with rectal evacuatory
dysfunction and rectal hyposensitivity. Ann Surg. 2012 Apr;255(4):643-9. doi:
10.1097/SLA.0b013e318247d49f. PMID: 22418005.
Leong RK, De Wachter SG, Nieman FH, de Bie RA, van Kerrebroeck PE. PNE versus 1st stage tined
lead procedure: a direct comparison to select the most sensitive test method to identify patients
suitable for sacral neuromodulation therapy. Neurourol Urodyn. 2011 Sep;30(7):1249-52. doi:
10.1002/nau.20979. Epub 2011 Mar 14. PMID: 21404317.
Leroi AM, Lenne X, Dervaux B, Chartier-Kastler E, Mauroy B, Normand LL, Grise P, Faucheron JL, Parc
Y, Lehur PA, Mion F, Damon H, Barth X, Leriche A, Saussine C, Guy L, Haab F, Bresler L, Sarramon JP,
Bensadoun H, Rullier E, Slim K, Sielezneff I, Mourey E, Ballanger P, Michot F. Outcome and cost analysis
of sacral nerve modulation for treating urinary and/or fecal incontinence. Ann Surg. 2011
Apr;253(4):720-32. doi: 10.1097/SLA.0b013e318210f1f4. PMID: 21475012.
Liberman D, Valiquette L. Concerns regarding sacral neuromodulation as a treatment option for
medical-refractory overactive bladder. Can Urol Assoc J. 2011 Aug; 5(4):285–7. doi:
10.5489/cuaj.11043. PMID: 21801689.
Maeda Y, Kamm MA, Vaizey CJ, Matzel KE, Johansson C, Rosen H, Baeten CG, Laurberg S. Long-term
outcome of sacral neuromodulation for chronic refractory constipation. Tech Coloproctol. 2017
Apr;21(4):277-286. doi: 10.1007/s10151-017-1613-0. Epub 2017 Apr 20. PMID: 28429130.
Martellucci J, Naldini G, Carriero A. Sacral nerve modulation in the treatment of chronic pelvic pain. Int
J Colorectal Dis. 2012 Jul;27(7):921-6. doi: 10.1007/s00384-011-1394-2. Epub 2011 Dec 29. PMID:
22203519.

Sacral Nerve Stimulation (Including Peripheral Nerve Stimulation Test and Two-Stage Tined Lead Procedure)
for Incontinence and Urinary Conditions
14 of 22
Martellucci J, Valeri A. Colonic electrical stimulation for the treatment of slow-transit constipation: a
preliminary pilot study. Surg Endosc. 2014 Feb;28(2):691-7. doi: 10.1007/s00464-013-3192-0. Epub
2013 Sep 19. PMID: 24048815.
Maternik M, Krzeminska K, Zurowska A. The management of childhood urinary incontinence. Pediatr
Nephrol. 2015 Jan;30(1):41-50. doi: 10.1007/s00467-014-2791-x. Epub 2014 Mar 11. PMID: 24615564.
Medtronic. Healthcare Professionals. InterStim™ System.
Mehmood S, Altaweel WM. Long-term outcome of sacral neuromodulation in patients with idiopathic
nonobstructive urinary retention: Single-center experience. Urol Ann. 2017 Jul-Sep;9(3):244–248.
doi: 10.4103/UA.UA_165_16. PMID: 28794590.
Mellgren A, Wexner SD, Coller JA, Devroede G, Lerew DR, Madoff RD, Hull T. Long-term efficacy and
safety of sacral nerve stimulation for fecal incontinence. Dis Colon Rectum. 2011 Sep;54(9):1065-75.
doi: 10.1097/DCR.0b013e31822155e9. PMID: 21825885.
Meyer I, Richter HE. An Evidence-Based Approach to the Evaluation, Diagnostic Assessment and
Treatment of Fecal Incontinence in Women. Curr Obstet Gynecol Rep. Author manuscript; available in
PMC 2014 Dec 8. Published in final edited form as: Curr Obstet Gynecol Rep. 2014 Sep;3(3):155–64.
doi: 10.1007/s13669-014-0085-8. PMID: 25505643.
Monga AK, Tracey MR, Subbaroyan J. A systematic review of clinical studies of electrical stimulation for
treatment of lower urinary tract dysfunction. Int Urogynecol J. 2012 Aug;23(8):993-1005. doi:
10.1007/s00192-012-1691-5. Epub 2012 Mar 17. PMID: 22426872.
Moya P, Arroyo A, Lacueva J, Candela F, Soriano-Irigaray L, López A, Gómez MA, Galindo I, Calpena R.
Sacral nerve stimulation in the treatment of severe faecal incontinence: long-term clinical, manometric
and quality of life results. Tech Coloproctol. 2014 Feb;18(2):179-85. doi: 10.1007/s10151-013-1022-y.
Epub 2013 Apr 27. PMID: 23624794.
National Institute for Health and Care Excellence (NICE). Faecal incontinence in adults: management.
Clinical Guideline CG49. 2007 Jun 27.
National Institute for Health and Care Excellence (NICE). Lower urinary tract symptoms in men:
management. Clinical Guideline CG97. 2010 May 23. Last Updated 2015 Jun 3.
National Institute for Health and Care Excellence (NICE). Urinary incontinence in neurological disease:
assessment and management. Clinical Guideline CG148. 2012 Aug 8.
National Institute for Health and Care Excellence (NICE). Urinary incontinence and pelvic organ
prolapse in women: management. NICE Guideline NG123. 2019 Apr 2. Last Updated 2019 Jun 24.
Nepple KG, Cooper CS. Management of bladder dysfunction in children. UpToDate. 2021 Jun 22.

Sacral Nerve Stimulation (Including Peripheral Nerve Stimulation Test and Two-Stage Tined Lead Procedure)
for Incontinence and Urinary Conditions
15 of 22
New Hampshire Department of Health and Human Services. Billing Manuals.
New Hampshire Department of Health and Human Services. Provider Notices.
Noblett KL, Cadish LA. Sacral nerve stimulation for the treatment of refractory voiding and bowel
dysfunction. Am J Obstet Gynecol. 2014 Feb;210(2):99-106. doi: 10.1016/j.ajog.2013.07.025. Epub 2013
Jul 27. PMID: 23899452.
Noblett K, Siegel S, Mangel J, Griebling TL, Sutherland SE, Bird ET, Comiter C, Culkin D, Bennett J,
Zylstra S, Kan F, Berg KC. Results of a prospective, multicenter study evaluating quality of life, safety,
and efficacy of sacral neuromodulation at twelve months in subjects with symptoms of overactive
bladder. Neurourol Urodyn. 2016 Feb;35(2):246-51. doi: 10.1002/nau.22707. Epub 2014 Dec 24.
PMID: 25546568.
Pilkington SA, Emmett C, Knowles CH, Mason J, Yiannakou Y; NIHR CapaCiTY working group; Pelvic
floor Society. Surgery for constipation: systematic review and practice recommendations: Results V:
Sacral Nerve Stimulation. Colorectal Dis. 2017 Sep;19 Suppl 3:92-100. doi: 10.1111/codi.13780. PMID:
28960926.
Sanford MT, Suskind AM. Neuromodulation in neurogenic bladder. Transl Androl Urol. 2016
Feb;5(1):117–26. doi: 10.3978/j.issn.2223-4683.2015.12.01. PMID: 26904417.
Schober MS, Sulkowski JP, Lu PL, Minneci PC, Deans KJ, Teich S, Alpert SA. Sacral nerve stimulation
for pediatric lower urinary tract dysfunction: development of a standardized pathway
with objective urodynamic outcomes. J Urol. 2015 Dec;194(6):1721-6. doi: 10.1016/j.juro.2015.06.090.
Epub 2015 Jun 30. PMID: 26141849.
Siegel S, Noblett K, Mangel J, Griebling TL, Sutherland SE, Bird ET, Comiter C, Culkin D, Bennett
J, Zylstra S, Berg KC, Kan F, Irwin CP. Results of a prospective, randomized, multicenter study
evaluating sacral neuromodulation with InterStim therapy compared with standard medical therapy at
6-months in subjects with mild symptoms of overactive bladder. Neurourol Urodyn. 2015
Mar;34(3):224-30. doi: 10.1002/nau.22544. Epub 2014 Jan 10. PMID: 24415559.
Sukhu T, Kennelly MJ, Kurpad R. Sacral neuromodulation in overactive bladder: a review and current
perspectives. Res Rep Urol. 2016 Oct 26;8:193-199. doi: 10.2147/RRU.S89544. eCollection 2016.. PMID:
27822462.
Sulkowski JP, Nacion KM, Deans KJ, Minneci PC, Levitt MA, Mousa HM, Alpert SA, Teich S. Sacral
nerve stimulation: a promising therapy for fecal and urinary incontinence and constipation in children. J
Pediatr Surg. 2015 Oct;50(10):1644-7. doi:10.1016/j.jpedsurg.2015.03.043. Epub 2015 Mar 26. PMID:
25858097.

Sacral Nerve Stimulation (Including Peripheral Nerve Stimulation Test and Two-Stage Tined Lead Procedure)
for Incontinence and Urinary Conditions
16 of 22
Tan E, Ngo NT, Darzi A, Shenouda M, Tekkis PP. Meta-analysis: sacral nerve stimulation versus
conservative therapy in the treatment of fecal incontinence. Int J Colorectal Dis. 2011 Mar;26(3):275-
94. doi: 10.1007/s00384-010-1119-y. Epub 2011 Jan 29. PMID: 21279370.
Thaha MA, Abukar AA, Thin NN, Ramsanahie A, Knowles CH. Sacral nerve stimulation for faecal
incontinence and constipation in adults. Cochrane Database Syst Rev. 2015 Aug 24;(8):CD004464.
doi: 10.1002/14651858.CD004464.pub3. PMID: 26299888.
Thin NN, Horrocks EJ, Hotouras A, Palit S, Thaha MA, Chan CL, Matzel KE, Knowles CH. Systematic
review of the clinical effectiveness of neuromodulation in the treatment of faecal incontinence. Br J
Surg. 2013 Oct;100(11):1430-47. doi: 10.1002/bjs.9226. PMID: 24037562.
Tirlapur SA, Vlismas A, Ball E, Khan KS. Nerve stimulation for chronic pelvic pain and bladder pain
syndrome: a systematic review. Acta Obstet Gynecol Scand. 2013 Aug;92(8):881-7. doi:
10.1111/aogs.12184. Epub 2013 Jun 22. PMID: 23710833.
Tutolo M, Ammirati E, Heesakkers J, Kessler TM, Peters KM, Rashid T, Sievert KD, Spinelli M, Novara G,
Van der Aa F, De Ridder D. Efficacy and Safety of Sacral and Percutaneous Tibial Neuromodulation in
Non-neurogenic Lower Urinary Tract Dysfunction and Chronic Pelvic Pain: A Systematic Review of the
Literature. Eur Urol. 2018 Mar;73(3):406-418. doi: 10.1016/j.eururo.2017.11.002. Epub 2018 Jan 12. PMID:
29336927.
U.S. Food and Drug Administration (FDA). Clinical Investigations of Devices Indicated for the
Treatment of Urinary Incontinence – Guidance for Industry and FDA Staff. 2011 Mar 8.
U. S. Food and Drug Administration (FDA). Medical Devices. 510(k) Clearances.
U. S. Food and Drug Administration (FDA). Medical Devices. Device Registration and Listing.
U.S. Food and Drug Administration (FDA). Summary of Safety and Effectiveness Data (SSED).
Implantable Electrical Stimulator for Incontinence. Medtronic® InterStim® Therapy System. Premarket
Approval Application (PMA) Number P080025. 2011 Mar 14.
Valentini FA, Marti BG, Robain G, Nelson PP. Phasic or terminal detrusor overactivity in women: age,
urodynamic findings and sphincter behavior relationships. Int Braz J Urol. 2011 Nov-Dec;37(6):773-80.
doi.org/10.1590/S1677-55382011000600014. PMID: 22233983.
van der Wilt AA, van Wunnik BP, Sturkenboom R, Han-Geurts IJ, Melenhorst J, Benninga MA, Baeten
CG, Breukink SO. Sacral neuromodulation in children and adolescents with chronic constipation
refractory to conservative treatment. Int J Colorectal Dis. 2016 Aug;31(8):1459-66. doi:
10.1007/s00384-016-2604-8. Epub 2016 Jun 13. PMID: 27294660.
Van Kerrebroeck PE, Marcelissen TA. Sacral neuromodulation for lower urinary tract dysfunction. 2012
Aug;30(4):445-50. doi: 10.1007/s00345-011-0780-2. Epub 2011 Oct 12. PMID: 21989816.
Sacral Nerve Stimulation (Including Peripheral Nerve Stimulation Test and Two-Stage Tined Lead Procedure)
for Incontinence and Urinary Conditions
17 of 22
Wald A. Diagnosis and Management of Fecal Incontinence. Curr Gastroenterol Rep. 2018 Mar
26;20(3):9. doi: 10.1007/s11894-018-0614-0. PMID: 29582182.
Wein AJ, Kavoussi LR, Partin AW, Peters CA. Campbell-Walsh Urology. 11th Edition. Elsevier. 2015 Nov
5.
Wexner SD, Coller JA, Devroede G, Hull T, McCallum R, Chan M, Ayscue JM, Shobeiri AS, Margolin
D, England M, Kaufman H, Snape WJ, Mutlu E, Chua H, Pettit P, Nagle D, Madoff RD, Lerew DR,
Mellgren A. Sacral nerve stimulation for fecal incontinence: results of a 120-patient prospective
multicenter study. Ann Surg. 2010 Mar;251(3):441-9. doi: 10.1097/SLA.0b013e3181cf8ed0. PMID:
20160636.
Whitehead WE, Rao SS, Lowry A, Nagle D, Varma M, Bitar KN, Bharucha AE, Hamilton FA. Treatment of
fecal incontinence: state of the science summary for the National Institute of Diabetes and Digestive
and Kidney Diseases workshop. Am J Gastroenterol. 2015 Jan;110(1):138-46; quiz 147. doi:
10.1038/ajg.2014.303. Epub 2014 Oct 21. PMID: 25331348.
Zerbib F, Siproudhis L, Lehur PA, Germain C, Mion F, Leroi AM, Coffin B, Le Sidaner A, Vitton V,
Bouyssou-Cellier C, Chene G; CONSTIMOD study investigators. Randomized clinical trial of sacral
nerve stimulation for refractory constipation. Br J Surg. 2017 Feb;104(3):205-213. doi:
10.1002/bjs.10326. Epub 2016 Oct 25. PMID: 27779312.
Next Review Date
09/01/23
Authorizing Entity
MPCTAC
Appendix
Appendix: Policy History
Disclaimer Information: +
Medical Policies are the Plan’s guidelines for determining the medical necessity of certain services or supplies for
purposes of determining coverage. These Policies may also describe when a service or supply is considered
experimental or investigational, or cosmetic. In making coverage decisions, the Plan uses these guidelines and
other Plan Policies, as well as the Member’s benefit document, and when appropriate, coordinates with the
Member’s health care Providers to consider the individual Member’s health care needs.
Plan Policies are developed in accordance with applicable state and federal laws and regulations, and accrediting
organization standards (including NCQA). Medical Policies are also developed, as appropriate, with consideration
of the medical necessity definitions in various Plan products, review of current literature, consultation with
practicing Providers in the Plan’s service area who are medical experts in the particular field, and adherence to
FDA and other government agency policies. Applicable state or federal mandates, as well as the Member’s
Sacral Nerve Stimulation (Including Peripheral Nerve Stimulation Test and Two-Stage Tined Lead Procedure)
for Incontinence and Urinary Conditions
18 of 22
benefit document, take precedence over these guidelines. Policies are reviewed and updated on an annual basis,
or more frequently as needed. Treating providers are solely responsible for the medical advice and treatment of
Members.
The use of this Policy is neither a guarantee of payment nor a final prediction of how a specific claim(s) will be
adjudicated. Reimbursement is based on many factors, including member eligibility and benefits on the date of
service; medical necessity; utilization management guidelines (when applicable); coordination of benefits;
adherence with applicable Plan policies and procedures; clinical coding criteria; claim editing logic; and the
applicable Plan – Provider agreement.
Sacral Nerve Stimulation (Including Peripheral Nerve Stimulation Test and Two-Stage Tined Lead Procedure)
for Incontinence and Urinary Conditions
19 of 22
Appendix: Policy History
Original Approval Date
Original Effective
Date* and Version
Number
Policy Owner
Original Policy
Approved by
Regulatory Approval:
N/A
Internal Approval:
10/03/06
12/03/06
Version 1
Director of Medical Policy
as Chair of Medical
Policy, Criteria, and
Technology Assessment
Committee (MPCTAC)
Quality and Clinical
Management Committee
(Q&CMC)
*Effective Date for QHP Commercial Product: 01/01/12
*Effective Date for New Hampshire Medicaid Product: 01/01/13
*Effective Date for Senior Care Options Product: 01/01/16
*Effective Date for New Hampshire Medicare Advantage HMO Product: 01/01/22
Note: Effective 05/01/13, this policy replaced Pelvic Floor/Sacral Nerve Stimulation for Urinary Incontinence
policy, policy number OCA 3.56, to include the medical necessity criteria for implantable sacral nerve stimulation
and the policy title was changed to Sacral Nerve Stimulation (Including Peripheral Nerve Stimulation Test and
Two-Stage Tined Lead Procedure) for Incontinence and Urinary Conditions.
Policy Revisions History
Review Date
Summary of Revisions
Revision
Effective Date
and Version
Number
Approved by
09/11/07
Updated template and added coding.
Version 2
09/11/07: MPCTAC
09/25/07: Utilization
Management Committee
(UMC)
10/15/07: Quality
Improvement Committee
(QIC)
09/09/08
No changes.
Version 3
09/09/08: MPCTAC
09/30/08: UMC
10/22/08: QIC
09/22/09
Updated references. No changes to
criteria.
Version 4
09/22/09: MPCTAC
10/28/09: QIC
09/01/10
Updated template and references. No
changes to criteria.
Version 5
10/20/10: MPCTAC
11/22/10: QIC
10/01/11
Updated limitations to include that sacral
nerve stimulation for the treatment of
fecal incontinence and posterior tibial
nerve stimulation for the treatment of
symptoms associated with overactive
bladder are considered experimental and
Version 6
10/19/11: MPCTAC
11/29/11: QIC
Sacral Nerve Stimulation (Including Peripheral Nerve Stimulation Test and Two-Stage Tined Lead Procedure)
for Incontinence and Urinary Conditions
20 of 22
Policy Revisions History
investigational. Updated references and
coding.
07/20/12
Off cycle review for Well Sense Health
Plan: Updated title, revised Summary
statement, added posterior tibial
stimulation to Description of Item or
Service, reformatted Medical Policy
Statement, updated Definitions, revised
language in Applicable Coding section,
updated code list.
Version 7
08/13/12: MPCTAC
09/13/12: QIC
12/01/12
Review for effective date 05/0/13.
Separated pelvic floor electrical
stimulation, implantable sacral nerve
stimulation, and posterior tibial nerve
stimulation into three separate policies;
policy formerly titled Pelvic Floor/Sacral
Nerve Stimulation for Urinary Incontinence
(formerly OCA: 3.65). Revised title and re-
numbered policy. Updated language in
Summary, Description of Item or Service,
Definitions, Applicable Coding, and Clinical
Background Information sections.
Reformatted criteria in Medical Policy
Statement section and added criteria for
peripheral nerve stimulation test and two-
stage tined lead procedure, updated
references, and added limitations. Revised
applicable code list. Referenced the
following policies: Experimental and
Investigational Treatment, Non-
Implantable Pelvic Floor Electrical
Stimulation for Urinary Incontinence,
Posterior Tibial Nerve Stimulation, and
Biofeedback for Urinary Incontinence.
Changed name of policy category from
“Clinical Coverage Guidelines” to “Medical
Policy.”
05/01/13
Version 8
12/19/12: MPCTAC
01/31/13: QIC
12/01/13:
Review for effective date 02/01/14.
Revised Description of Item or Service
section. Reformatted Medical Policy
Statement section without changing
criteria. Updated code definitions without
changing applicable code list. Updated
references.
02/01/14
Version 9
12/18/13: MPCTAC
01/21/14: QIC
12/01/14
Review for effective date 02/01/15.
Updated references.
02/01/15
Version 10
12/17/14: MPCTAC
01/14/15: QIC
Sacral Nerve Stimulation (Including Peripheral Nerve Stimulation Test and Two-Stage Tined Lead Procedure)
for Incontinence and Urinary Conditions
21 of 22
Policy Revisions History
10/01/15
Review for effective date 12/01/15.
Updated template with list of applicable
products and corresponding notes.
12/01/15
Version 11
10/21/15: MPCTAC
11/11/15: QIC
10/21/15
Review for effective date 02/01/16.
Revised limitations. Updated References,
Definitions, and Clinical Background
Information sections.
02/01/16
Version 12
10/21/15: MPCTAC
11/11/15: QIC
11/25/15
Review for effective date 02/01/16.
Revised language in the Applicable Coding
section.
02/01/16
Version 13
11/25/15: MPCTAC
(electronic vote)
12/09/15: QIC
10/01/16
Review for effective date 12/01/16.
Administrative changes made to the
Summary, Medical Policy Statement,
Definitions, Clinical Background
Information, References, and References
to Applicable Laws and Regulations
sections. No change to criteria or
applicable code list.
12/01/16
Version 14
10/19/16: MPCTAC
11/09/16: QIC
10/01/17
Review for effective date 01/01/18.
Administrative changes made to the Policy
Summary, Description of Item or Service,
Definitions, Clinical Background
Information, References, and Other
Applicable Policies sections. Criteria
revised in the Medical Policy Statement
and Limitations sections.
01/01/18
Version 15
10/24/17: MPCTAC
(electronic vote)
10/01/18
Review for effective date 01/01/19.
Administrative changes made to the Policy
Summary, Description of Item or Service,
Definitions, Clinical Background
Information, References, and Other
Applicable Policies sections. Revised
criteria in the Medical Policy Statement
and Limitations sections.
01/01/19
Version 16
10/17/18: MPCTAC
09/01/19
Review for effective date 10/01/19.
Administrative changes made to the
Clinical Background Information,
References, Other Applicable Policies, and
Reference to Applicable Laws and
Regulations sections. Revised Plan notes
in the Applicable Coding section.
10/01/19
Version 17
09/18/19: MPCTAC
09/01/20
Review for effective date 10/01/20.
Administrative changes made to the
References and Other Applicable Policies
sections.
10/01/20
Version 18
09/16/20: MPCTAC
Sacral Nerve Stimulation (Including Peripheral Nerve Stimulation Test and Two-Stage Tined Lead Procedure)
for Incontinence and Urinary Conditions
22 of 22
Policy Revisions History
10/01/21
Review for effective date 01/01/22.
Adopted new medical policy template;
removed administrative sections, Medical
Policy Statement section renamed Clinical
Criteria section, and Limitations section
renamed Limitations and Exclusions
section. Added NH Medicare Advantage
HMO as an applicable product effective
01/01/22. Administrative changes made to
the Policy Summary, Limitations and
Exclusions, Applicable Coding, and
References sections. Criteria revised in
the Clinical Criteria section.
01/01/22
Version 19
Not
implemented -
replaced with
Version 20
10/20/21: MPCTAC
12/01/21
Review for effective date 01/01/22.
Industry-wide code description change in
the Applicable Coding section. Revisions
approved in version 19 implemented.
01/01/22
Version 20
Not applicable because
industry-wide code
description change;
12/15/21: MPCTAC review
09/01/22
Review for effective date 12/01/22.
Administrative changes to Policy
Summary, Clinical Criteria, Limitations and
Exclusions, and References sections. ICD-
10 diagnosis codes for fecal or urinary
incontinence added to be billed in
combination with CPT/HCPCS procedure
codes in the Applicable Coding section.
12/01/22
Version 21
09/23/22: MPCTAC
(electronic vote)
Speech Therapy, Language Therapy, Voice Therapy, or Auditory Rehabilitation in the Outpatient Setting (NH Products)
1 of 10
Medical Policy – Policy with InterQual Criteria Retired and AIM Criteria Adopted as of 12/01/22
Speech Therapy, Language Therapy, Voice Therapy, or Auditory
Rehabilitation in the Outpatient Setting
Policy Number: OCA 3.542
Version Number: 33
Policy Retired Date: 12/01/22
Impacted Products
☐ All Products
☒ NH Medicaid
☒ NH Medicare Advantage
☐ MA MassHealth ACO
☐ MA MassHealth MCO
☐ MA Qualified Health Plans/Employer Choice Direct
☐ MA Senior Care Options
Note: Disclaimer and audit information is located at the end of this document.
Policy Summary
The Plan considers outpatient speech therapy (i.e., speech and language therapy, swallowing therapy,
feeding therapy, aural or auditory rehabilitation, and/or voice therapy) medically necessary, including
habilitative services and/or rehabilitative services, when AIM clinical appropriateness guidelines are
met for an adult or pediatric member or are required EPSDT services for a member age 20 or younger
on the date of service. Prior authorization from AIM Specialty Health is required for outpatient speech
therapy (ST) after the initial evaluation. ST must be provided within the scope of practice of the
treating professional and/or paraprofessional and follow all applicable state licensing and supervisory
requirements.
Clinical Criteria
No medical policy criteria.
Limitations and Exclusions
None.
Speech Therapy, Language Therapy, Voice Therapy, or Auditory Rehabilitation in the Outpatient Setting (NH Products)
2 of 10
Variations
The Plan uses guidance from the Centers for Medicare & Medicaid Services (CMS) for medical
necessity and coverage determinations for Plan’s New Hampshire Medicare Advantage HMO
members, including but not limited to national coverage determinations (NCDs), local coverage
determinations (LCDs), local coverage articles (LCAs), and documentation included in Medicare
manuals. At the time of the Plan’s most recent policy review, no applicable clinical guidelines were
found from CMS. Verify CMS criteria in effect for the requested service on the date of the prior
authorization request for a NH Medicare Advantage HMO member. When there is no guidance from
CMS for the requested service for the specified indication on the date of the prior authorization
request, Plan-adopted clinical review criteria will be used to determine the medical necessity of the
service.
Applicable Coding
The Plan utilizes up-to-date, industry-standard Current Procedural Terminology (CPT) codes, Health
Care Common Procedure Coding System (HCPCS) codes, and International Statistical Classification
of Diseases and Related Health Problems, 10th revision (ICD-10) diagnosis codes in the Plan’s medical
policies. The list of applicable codes included in this policy is informational only and may not be all
inclusive. Applicable codes are subject to change without prior notification and do not guarantee
member coverage or provider reimbursement. Review the Plan’s reimbursement policies for Plan
billing guidelines. Providers are responsible for obtaining prior authorization from AIM for speech
therapy, even if an applicable code appropriately describing the service is not included in this policy’s
Applicable Coding section. Providers are expected to report all services using the most up-to-date,
industry-standard procedures and diagnosis codes at the time of the service.
CPT Codes
Code Descriptions
92507
Treatment of speech, language, voice, communication, and/or auditory
processing disorder; individual
92508
Treatment of speech, language, voice, communication, and/or auditory
processing disorder; group, two or more individuals
92526
Treatment of swallowing dysfunction and/or oral function for feeding
92606
Therapeutic services for use of non-speech-generating device with programming
92609
Therapeutic services for use of speech-generating device with programming
97129
Therapeutic interventions that focus on cognitive function (e.g., attention, memory,
reasoning, executive function, problem solving, and/or pragmatic functioning) and
compensatory strategies to manage the performance of an activity (e.g., managing time or
schedules, initiating, organizing, and sequencing tasks), direct (one-on-one) patient
contact; initial 15 minutes
97130
Therapeutic interventions that focus on cognitive function (e.g., attention, memory,
reasoning, executive function, problem solving, and/or pragmatic functioning) and
compensatory strategies to manage the performance of an activity (e.g., managing time or
schedules, initiating, organizing, and sequencing tasks), direct (one-on-one) patient
contact; each additional 15 minutes (List separately in addition to code for primary
procedure)

Speech Therapy, Language Therapy, Voice Therapy, or Auditory Rehabilitation in the Outpatient Setting (NH Products)
3 of 10
References
American Academy of Otolaryngology - Head and Neck Surgery Foundation (AAO-HNSF). Clinical
Practice Guidelines.
American Academy of Otolaryngology - Head and Neck Surgery Foundation (AAO-HNSF). Schwartz
S, Cohen S, Dailey S, Rosenfeld R, Deutsch E, Gillespie B, Granieri E, Hapner E, Kimball E, Krouse H,
McMurray S, Medina S, O'Brien K, Ouellette D, Messinger-Rapport B, Stachler R, Strode S, Thompson
D, Stemple J, Willging P, Cowley T, McCoy, Bernad P, Patel M. Clinical practice guideline: hoarseness
(dysphonia). Otolaryngol Head Neck Surg. 2009 Sep;141(3S2):S1-31. doi: 10.1016/
j.otohns.2009.06.744. PMID: 19729111.
American Academy of Otolaryngology - Head and Neck Surgery Foundation (AAO-HNSF). Stachler
RJ, Francis DO, Schwartz SR, Damask CC, Digoy GP, Krouse HJ, McCoy SJ, Ouellette DR, Patel RR,
Reavis CCW, Smith LJ, Smith M, Strode SW, Woo P, Nnacheta LC. Clinical Practice Guideline:
Hoarseness (Dysphonia) (Update). Otolaryngol Head Neck Surg. 2018 Mar;158(1_suppl):S1-S42. doi:
10.1177/0194599817751030. PMID: 29494321.
American Speech-Language-Hearing Association (ASHA). Adult Speech and Language.
American Speech-Language-Hearing Association (ASHA). Cognitive-Communication. ASHA Policy
Documents.
American Speech-Language-Hearing Association (ASHA). Scope of Practice in Speech-Language
Pathology.
American Speech-Language-Hearing Association (ASHA). Speech-Language Pathology Medical
Review Guidelines.
American Speech-Language-Hearing Association (ASHA). Stuttering.
American Speech-Language-Hearing Association (ASHA). Swallowing and Feeding Disorders.
Bahar-Fuchs A, Clare L, Woods B. Cognitive training and cognitive rehabilitation for persons with mild
to moderate dementia of the Alzheimer's or vascular type: a review. Alzheimers Res Ther. 2013;5(4):35.
doi: 10.1186/alzrt189. PMID: 23924584.
Centers for Medicare & Medicaid Services (CMS). Local Coverage Determination (LCD) L33580.
Speech-Language Pathology. 2015 Oct 1. National Governmental Services, Inc. 2015 Dec 19. Revision
Effective Date 2019 Dec 19.

Speech Therapy, Language Therapy, Voice Therapy, or Auditory Rehabilitation in the Outpatient Setting (NH Products)
4 of 10
Centers for Medicare & Medicaid Services (CMS). Manuals. Publication # 100-02. Medicare Benefit
Policy Manual.
Centers for Medicare & Medicaid Services (CMS). Manuals. Publication # 100-03. Medicare National
Coverage Determinations (NCD) Manual.
Centers for Medicare & Medicaid Services (CMS). Medicare Coverage Database (MCD).
Centers for Medicare & Medicaid Services (CMS). National Coverage Determination (NCD) 170.3.
Speech-Language Pathology Services for the Treatment of Dysphagia. 2006 Oct 1.
Centers for Medicare & Medicaid Services (CMS). Transmittals.
Hauser RA. What is the Lee Silverman Voice Treatment (LSVT) program for Parkinson disease (PD)?
Medscape. 2019 Aug 29.
Hayes. Health Technology Assessment. Cognitive Rehabilitation Therapy for Traumatic Brain Injury
(TBI). Dallas, TX: Hayes; 2017 Sep 26. Annual Review 2021 Feb 8.
Hayes. Health Technology Assessment. Lee Silverman Voice Treatment (LSVT) LOUD for Speech and
Voice Problems in Parkinson Disease. Dallas, TX: Hayes; 2020 Nov 9.
New Hampshire Department of Health and Human Services. Billing Manuals.
New Hampshire Department of Health and Human Services. NH Medicaid Program.
New Hampshire Department of Health and Human Services. Provider Notices.
New Hampshire Medicaid. Therapies. Physical, Occupational, Speech. Provider Manual. Volume II. 2017
Dec 1.
New Hampshire Office of Professional Licensure and Certification. Office of Licensed Allied Health
Professionals. Laws and Administrative Rules Governing Licensed Allied Health Professionals.
Next Review Date
Not applicable
Retired Date
12/01/22

Speech Therapy, Language Therapy, Voice Therapy, or Auditory Rehabilitation in the Outpatient Setting (NH Products)
5 of 10
Authorizing Entity
MPCTAC
Appendix
Appendix: Policy History
Disclaimer Information:
Plan refers to Boston Medical Center Health Plan, Inc. which operates under the trade name WellSense Health Plan. Medical
Policies are the Plan’s guidelines for determining the medical necessity of certain services or supplies for purposes of
determining coverage. These Policies may also describe when a service or supply is considered experimental or
investigational, or cosmetic. In making coverage decisions, the Plan uses these guidelines and other Plan Policies, as well as
the Member’s benefit document, and when appropriate, coordinates with the Member’s health care Providers to consider the
individual Member’s health care needs.
Plan Policies are developed in accordance with applicable state and federal laws and regulations, and accrediting organization
standards (including NCQA). Medical Policies are also developed, as appropriate, with consideration of the medical necessity
definitions in various Plan products, review of current literature, consultation with practicing Providers in the Plan’s service
area who are medical experts in the particular field, and adherence to FDA and other government agency policies. Applicable
state or federal mandates, as well as the Member’s benefit document, take precedence over these guidelines. Policies are
reviewed and updated on an annual basis, or more frequently as needed. Treating providers are solely responsible for the
medical advice and treatment of Members.
The use of this Policy is neither a guarantee of payment nor a final prediction of how a specific claim(s) will be adjudicated.
Reimbursement is based on many factors, including member eligibility and benefits on the date of service; medical necessity;
utilization management guidelines (when applicable); coordination of benefits; adherence with applicable Plan policies and
procedures; clinical coding criteria; claim editing logic; and the applicable Plan – Provider agreement.
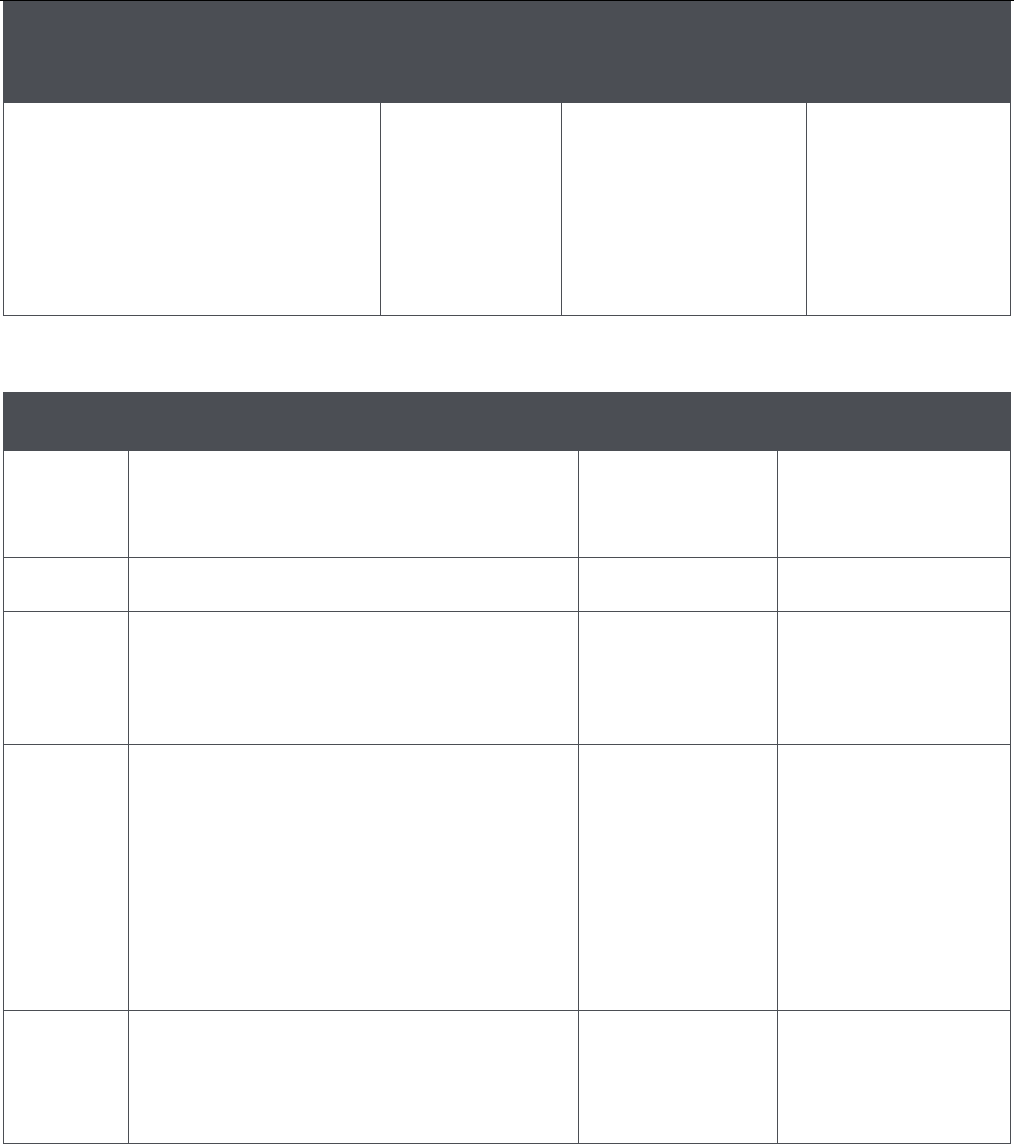
Speech Therapy, Language Therapy, Voice Therapy, or Auditory Rehabilitation in the Outpatient Setting (NH Products)
6 of 10
Appendix: Policy History
Original
Approval Date
Original
Effective Date*
and Version
Policy Owner
Original Policy
Approved by
Regulatory Approval: N/A
Internal Approval:
03/16/11: Medical Policy, Criteria, and
Technology Assessment Committee
(MPCTAC)
04/27/11: Quality Improvement
Committee (QIC)
07/01/11
Version 1
Director of Medical
Policy as Chair of
Medical Policy, Criteria,
and Technology
Assessment Committee
(MPCTAC)
MPCTAC and QIC
* Effective Date for NH Medicaid Product: 01/01/13
* Effective Date for NH Medicare Advantage HMO Product: 01/01/22
Policy Revisions History
Review
Date
Summary of Revisions
Revision
Effective Date
and Version
Number
Approved by
03/19/12
Updated references.
Version 2
03/21/12: MPCTAC
04/25/12: QIC
08/01/12
Off cycle review. Revised Summary statement,
reformatted Medical Policy Statement, revised
Applicable Coding introductory paragraph,
updated code list, revised Limitations, and
updated references.
Version 3
08/13/12: MPCTAC
09/06/12: QIC
11/01/12
Review for effective date 03/01/13. Updated
references. Revised title so policy applies to
members age 22 or older (rather than members
over the age of 21). Added language in
Summary section to clarify text. Referenced
Plan reimbursement policy 4.609 for therapy
reimbursement guidelines. Reorganized clinical
criteria in Medical Policy Statement section and
referenced InterQual® criteria. Revised
applicable code list.
03/01/13
Version 4
11/21/12: MPCTAC
12/20/12: QIC
08/14/13
and
08/15/13
Off cycle review. Incorporate policy revisions
dated 11/01/12 (as specified above) for the New
Hampshire Medicaid product; these policy
revisions were approved by MPCTAC on
11/21/12 and QIC on 12/20/12 for applicable Plan
08/14/13: MPCTAC
(via electronic vote)
08/15/13: QIC
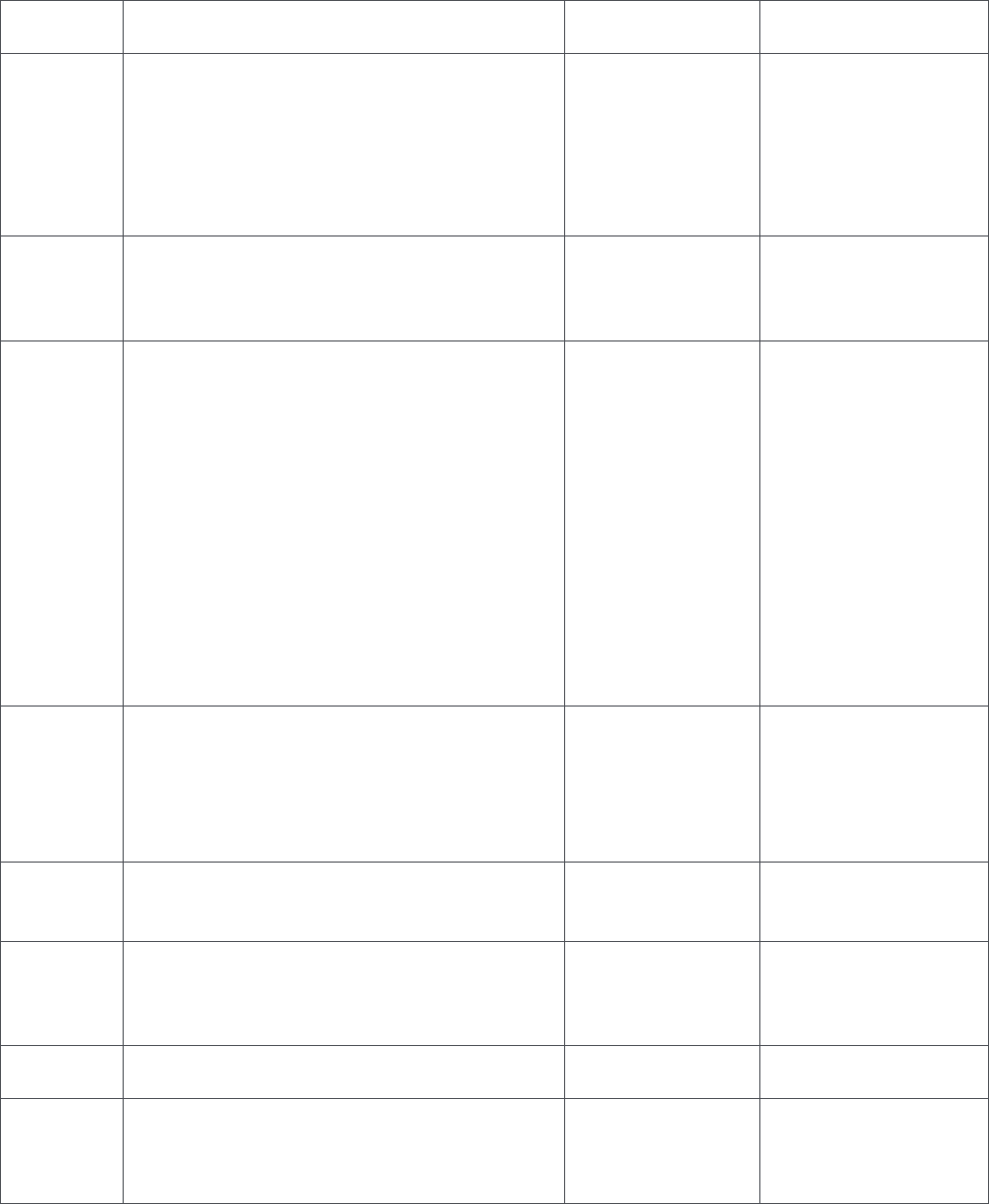
Speech Therapy, Language Therapy, Voice Therapy, or Auditory Rehabilitation in the Outpatient Setting (NH Products)
7 of 10
products. Additional review of policy
conducted.
11/01/13,
12/01/13,
01/01/14,
and
02/01/14
Review for effective date 05/01/14. Revised
Applicable Coding section by updating code
definitions and Plan notes, introductory
paragraph, and applicable codes for the
Massachusetts and New Hampshire products.
Reformatted Limitations section without
changing criteria. Updated references.
05/01/14
Version 5
02/11/14: MPCTAC
02/18/14: QIC
09/08/14
For New Hampshire products only, waive prior
authorization of first 2 treatment sessions per
member per servicing provider per calendar
year.
10/01/14
Version 11
Addendum A
09/17/14: MPCTAC
09/30/14: QIC
11/04/14
and
11/19/14
Review for effective date 01/11/15. Summary
and Medical Policy Statement sections updated
with guidelines specified in version 11,
addendum A. Policy renumbered OCA 3.542 to
include speech therapy (and associated
therapies) for members age 21 or older in the
outpatient setting for Well Sense Health Plan
members. Revised language in the Applicable
Coding section without changing the applicable
code list. Age range changed from age 22 or
older to age 21 or older for adult Well Sense
members; ST services for adult members
formerly in policy number OCA 3.551. Revised
review calendar.
01/11/15
Version 12
11/06/14: MPCTAC
(electronic vote)
11/11/14: QIC
(electronic vote)
11/19/14: MPCTAC
12/10/14: QIC
12/03/15
Review for effective date 01/01/16. Updated
template and Summary section. Administrative
changes made to the Medical Policy Statement
and Limitations sections without changing
criteria. Revised language in the Applicable
Coding section. Added definitions.
01/01/16
Version 13
12/03/15: MPCTAC
(electronic vote)
12/09/15: QIC
12/01/16
Review for effective date 02/01/17. Clarified
existing criteria in the Medical Policy Statement
section. Updated references.
02/01/17
Version 14
12/21/16: MPCTAC
01/11/17: QIC
05/01/17
Review for effective date 08/01/17. Removed
CPT code 92524 from the applicable code list
because it is an initial evaluation code for voice
and resonance.
08/01/17
Version 15
05/17/17: MPCTAC
12/01/17
Review for effective date 01/01/17. Updated
Policy Summary section.
01/01/17
Version 16
12/20/17: MPCTAC
12/01/17
Review for effective date 01/01/18. Industry-
wide updates to codes included in the
Applicable Coding section. Annual review of
policy with administrative changes made to the
01/01/18
Version 17
12/20/17: MPCTAC
Speech Therapy, Language Therapy, Voice Therapy, or Auditory Rehabilitation in the Outpatient Setting (NH Products)
8 of 10
Medical Policy Statement, Definitions, and
Reference sections.
02/01/18
Review for effective date 03/01/18.
Administrative changes made to the Policy
Summary and Limitations sections.
03/01/18
Version 18
02/21/18: MPCTAC
11/01/18
Review for effective date 12/01/18.
Administrative changes made to the
Limitations, Definitions, References, Other
Applicable Policies, and Reference to
Applicable Laws and Regulations sections.
12/01/18
Version 19
11/21/18: MPCTAC
03/01/19
Review for effective date 07/01/19.
Administrative changes made to the Limitations
and Reference to Applicable Laws and
Regulations sections. Criteria revised in the
Medical Policy Statement section.
07/01/19
Version 20
03/20/19: MPCTAC
05/01/19
Review for effective date 08/01/19. Revised
criteria in the Medical Policy Statement section.
Administrative changes made to the
References and Reference to Applicable Laws
and Regulations sections.
05/15/19
Version 21
05/15/19: MPCTAC
12/01/19
Review for effective date 01/01/20. Industry-
wide code deletion required revision to coding
in the Applicable Coding section.
01/01/20
Version 22
Not applicable because
industry-wide code
changes.
11/01/19
Review for effective date 02/01/20.
Administrative changes made to the Policy
Summary, References and Reference to
Applicable Laws and Regulations sections.
Criteria revised in the Medical Policy Statement
and Limitations sections.
02/01/20
Version 23
Renumbered to
Version 23 to
implement
industry-wide code
updates effective
01/01/20 in Version
22
11/20/19: MPCTAC
12/01/19
Review for effective 02/01/20. Industry-wide
code deletion required revision to coding in the
Applicable Coding section of the policy version
23 effective 02/01/20.
02/01/20
Version 24
Not applicable because
industry-wide code
changes.
12/01/19
Review for effective date 03/01/20. Revised in
the Medical Policy Statement section the
definition of a servicing ST provider for the prior
authorization waiver.
03/01/20
Version 25
12/18/19: MPCTAC
11/01/20
Review for effective date 02/01/21.
Administrative changes made to the Definitions,
Applicable Coding, and References sections.
Revised criteria in the Medical Policy Statement
section.
02/01/21
Version 26
11/18/20: MPCTAC
Speech Therapy, Language Therapy, Voice Therapy, or Auditory Rehabilitation in the Outpatient Setting (NH Products)
9 of 10
05/01/21
Review for effective date 08/01/21.
Administrative changes made to the Policy
Summary, Medical Policy Statement,
Limitations, Definitions, and References
sections. Codes added to the Applicable
Coding section.
08/01/21
Version 27
05/19/21: MPCTAC
10/01/21
Review for effective date 01/01/22 Adopted
new medical policy template; removed
administrative sections, Medical Policy
Statement section renamed Clinical Criteria
section, and Limitations section renamed
Limitations and Exclusions section.
Administrative changes made to the Policy
Summary, Limitations and Exclusions,
Applicable Coding, and References sections.
Added New Hampshire Medicare Advantage
HMO as an applicable product effective
01/01/22. Added gender dysphoria as a
medically necessary indication for voice therapy
in the Criteria section.
01/01/22
Version 28
10/20/21: MPCTAC
02/01/22
Review for effective date 02/01/22.
Administrative changes made to the Policy
Summary. Revised policy title because policy
will apply to adult and pediatric members.
Adopted InterQual criteria to determine
medical necessity and retired medical policy
criteria. Gender dysphoria specified as a
medically necessary indication for voice therapy
in the Gender Affirmation Services medical
policy, OCA 3.11, as of 01/01/22.
02/01/22
Version 29
11/17/21: MPCTAC
05/01/22
Review for effective date 06/01/22.
Administrative changes made to the Policy
Summary, Clinical Criteria, Limitations and
Exclusions, and Applicable Coding sections.
06/01/22
Version 30
05/11/22: MPCTAC
(electronic vote)
05/01/22
Review for effective date 08/01/22. Revised
code list in the Applicable Coding section.
08/01/22
Version 31
05/11/22: MPCTAC
08/01/22
Review for policy retired date 11/01/22.
Administrative changes made to the Policy
Summary and Applicable Coding sections.
InterQual medical necessity criteria and medical
policy guidelines in the Clinical Criteria and
Limitations and Exclusions sections retired on
11/01/22. AIM criteria adopted for outpatient ST
on 11/01/22. Plan prior authorization waivers
removed after 10/31/22. AIM prior
authorization is required for outpatient ST after
11/01/22
Version 32
Version 32 NOT
implemented;
Version 31 effective
08/01/22 to
11/30/22
08/26/22: MPCTAC
(electronic vote)
Speech Therapy, Language Therapy, Voice Therapy, or Auditory Rehabilitation in the Outpatient Setting (NH Products)
10 of 10
the initial evaluation as of 11/01/22, even when
applicable codes are not listed in this Plan
policy.
09/01/22
Review for policy retired date 12/01/22. The
effective date of AIM Specialty Health’s
management of outpatient rehabilitation
services changed from 11/01/22 to 12/01/22.
Administrative changes made to the Policy
Summary and Applicable Coding sections.
InterQual medical necessity criteria and medical
policy guidelines in the Clinical Criteria and
Limitations and Exclusions sections retired as of
12/01/22. AIM criteria adopted for outpatient
ST for dates of service on or after 12/01/22.
Plan prior authorization waivers removed after
11/30/22. AIM prior authorization is required for
outpatient ST after the initial evaluation as of
12/01/22, even when applicable codes are not
listed in this Plan policy.
12/01/22
Version 33
09/23/22: MPCTAC
(electronic vote)
Temporomandibular Joint Disorder Treatment
1 of 16
Medical Policy
Temporomandibular Joint Disorder Treatment
Policy Number: OCA 3.968
Version Number: 23
Version Effective Date: 11/01/22
Impacted Products
☒ All Products
☒ NH Medicaid
☒ NH Medicare Advantage
☒ MA MassHealth ACO
☒ MA MassHealth MCO
☒ MA Qualified Health Plans/Employer Choice Direct
☒ MA Senior Care Options
Note: Disclaimer and audit information is located at the end of this document.
Policy Summary
The Plan considers medical and/or surgical (non-dental) treatment of a temporomandibular joint
(TMJ) disorders to be medically necessary ONLY when the disorders are caused by, or results from a
specific medical condition. Examples of specific medical conditions include jaw fractures and/or
dislocations and degenerative arthritis. Plan prior authorization is required. Separate coverage is
outlined in the member’s benefit documents for dental services (if dental services are covered for the
Plan member). This medical policy ONLY includes guidelines for TMJ disorders related to a medical
condition for medical and/or surgical (non-dental) treatment.
For dates of service on or after November 1, 2022, the Plan uses AIM clinical appropriateness
guidelines to determine the medical necessity of radiology services, musculoskeletal services (i.e.,
spine surgeries, joint surgeries, and interventional pain management treatments) and genetic testing.
AIM manages outpatient rehabilitation services (i.e., physical therapy, occupational therapy, and
speech therapy) for Plan members for dates of service on or after December 1, 2022. Prior
authorization from AIM Specialty Health is required for these services.
Clinical Criteria
Criteria must be met in item A (medical necessity criteria) or item B (services that require Plan Medical
Director review):
Temporomandibular Joint Disorder Treatment
2 of 16
A. Criteria must be met in either item 1 or item 2:
1. Initial Medical Evaluation: Prior authorization is REQUIRED for the initial medical evaluation for
a TMJ disorder ONLY when conducted by a provider who is NOT a participating oral and
maxillofacial surgeon or participating otolaryngologist; OR
2. Treatment after the Initial Evaluation: All medical and/or surgical treatments for TMJ disorders
REQUIRE prior authorization after the initial medical evaluation. ALL criteria must be met in
items a through c:
a. Medical condition eligible for treatment includes ANY of the following:
(1) Jaw fracture or jaw dislocation (i.e., current fracture or acute dislocation); OR
(2) Degenerative arthritis; AND
b. Medical condition is confirmed by diagnostic x-rays or other generally accepted diagnostic
procedures used to diagnose a jaw fracture, jaw dislocation, and/or degenerative arthritis,
including but not limited to a CT scan, MRI, tomogram, or arthrogram; AND
c. Based on the treatment plan determined by the treating provider, the member requires
ANY treatment specified in item (1) or item (2):
(1) Criteria for Non-Surgical Treatment: Covered first-line, conservative treatment may
include diet and behavior modification and ANY combination of treatment listed below
in items (a) through (e):
(a) Pharmacologic therapy such as anti-inflammatory, muscle relaxants, and/or
analgesics (according to guidelines included in the Plan’s pharmacy policies and
fomulary applicable for the member’s benefit coverage); OR
(b) Occupational therapy, speech therapy, and/or physical therapy; OR
(c) Use of mandibular orthopedic repositioning appliances (MORA); OR
(d) Therapeutic injections (e.g. local anesthetic or corticosteroids); OR
(e) Manipulation for reduction of fracture or dislocation; OR
(2) Criteria for Surgical Treatment: ANY criteria must be met in items (a) through (e):
(a) Arthrocentesis (e.g., for acute closed lock); OR
(b) Arthroscopic surgery (e.g., for arthritis); OR

Temporomandibular Joint Disorder Treatment
3 of 16
(c) Intraoral vertical ramus osteotomy (IVRO) to correct internal derangements; OR
(d) Open surgical procedure such as open reduction, arthroplasty, condylectomy,
meniscus or disc plication, or disc removal; OR
(e) TMJ arthroplasty will be performed with an FDA-approved prosthetic implant
(only) according to the FDA-approved indication for the implantation.
B. Medical Director review is required for individual consideration when medical necessity criteria are
NOT met and/or the disorder may be caused by a medical condition other than a jaw fracture, jaw
dislocation, and/or degenerative arthritis.
Limitations and Exclusions
A. The treatment of TMJ disorders or TMJ syndrome that is NOT related to a medical condition
would be considered a dental service rather than a medical benefit.
B. ANY of the following services is considered NOT medically necessary for the assessment and/or
treatment of TMJ disorders or other TMJ-related indications:
1. Treatment of a TMJ disorder that is NOT proven to be caused by or to result in a specific
medical condition; OR
2. Acupuncture (unless a covered benefit for the member for the specified indication); OR
3. Arthroscopy of the TMJ for diagnostic purposes only; OR
4. Biofeedback; OR
5. Dental or orthodontic services (including restorations, prostheses procedures, radiographic
images, oral/facial photographic images, supplies) for TMJ-related indications and/or to adjust
the height of teeth or other way restore occlusion, such as crowns, bridges, braces; OR
6. Devices/appliances such as mechanical stretching devices or devices to maintain range of
motion, gain increased range of motion, and/or improve functioning of the TMJ, including but
not limited to continuous passive motion (CPM) devices, passive rehabilitation therapy devices,
mandibular orthopedic repositioning appliances (MORA); OR
7. Dry needling alone or in combination with a stretching regimen used to reduce pain and
increase range of motion in patients with TMJ pain; OR
8. Electrical stimulation techniques such as:
Temporomandibular Joint Disorder Treatment
4 of 16
a. Electrogalvanic stimulation; OR
b. Microcurrent electrical therapy (MET); OR
c. Percutaneous electrical stimulation (PENS); OR
d. Percutaneous neuromodulation therapy (e.g., the Percutaneous Neuromodulation
Therapy™ by Vertis Neurosciences system or the Deepwave® Percutaneous
Neuromodulation Pain Therapy System by Biowave Corp.); OR
e. Transcutaneous electrical nerve stimulation (TENS); OR
9. Electromyography (EMG); OR
10. Intra-articular injection of hyaluronic acid (viscosupplementation); OR
11. Iontophoresis using electricity to enhance the percutaneous absorption of a drug or chemical
ions (e.g., lidocaine hydrochloride, dexamethasone sodium phosphate); OR
12. Jaw tracking devices, computerized jaw tracking technologies, and associated jaw tracking
services using one or more technologies/services (e.g., TENS, 3D imaging/computerized
mandibular scans, kinesiography, magnetic recording devices, electronic motion recording
methods, and/or range of motion measurements); OR
13. Kinesiography; OR
14. Laser therapy; OR
15. Neuromuscular junction studies, range of motion measurements, and/or muscle testing; OR
16. Phonophoresis using ultrasound to enhance the delivery of topically applied drugs; OR
17. Somatosensory testing (also known as somatosensory evoked potentials test, SEPs, or SSEPs);
OR
18. Thermography (including digital infrared thermal imaging, magnetic resonance thermography
and temperature gradient studies); OR
19. Transcranial or lateral skull x-rays; OR
20. Ultrasonic Doppler auscultation/ultrasound imaging/sonogram for diagnosing disorders of the
temporomandibular joint; OR
Temporomandibular Joint Disorder Treatment
5 of 16
21. Use of a TMJ arthroplasty implant or device not FDA approved or not used according to FDA-
approved indications.
Variations
The Plan uses guidance from the Centers for Medicare & Medicaid Services (CMS) for medical
necessity and coverage determinations for the Plan’s Senior Care Options (SCO) members and New
Hampshire Medicare Advantage HMO members, including but not limited to national coverage
determinations (NCDs), local coverage determinations (LCDs), local coverage articles (LCAs), and
documentation included in Medicare manuals. At the time of the Plan’s most recent policy review, no
applicable clinical guidelines were found from CMS specifically for temporomandibular joint disorder,
but CMS guidelines do exist for services that may be used for the diagnosis or treatment of TMJ.
Verify CMS criteria in effect on the date of the prior authorization request. When there is no guidance
from CMS for the requested service for the specified indication on the date of the prior authorization
request, Plan-adopted clinical review criteria will be used to determine the medical necessity of the
service.
Applicable Coding
The Plan utilizes up-to-date, industry-standard Current Procedural Terminology (CPT) codes, Health
Care Common Procedure Coding System (HCPCS) codes, and International Statistical Classification
of Diseases and Related Health Problems, 10th revision (ICD-10) diagnosis codes in the Plan’s medical
policies. Since these codes may be updated at different intervals than the medical policy review cycle,
the list of applicable codes included in a policy is informational only and may not be all
inclusive. Applicable codes are subject to change without prior notification and do not guarantee
member coverage or provider reimbursement. Review the Plan’s reimbursement policies for Plan
billing guidelines. Providers are responsible for obtaining prior authorization for the services specified
in the Clinical Criteria section and Limitations and Exclusions section of a medical policy, even if an
applicable code appropriately describing the service is not included in the policy’s Applicable Coding
section. Providers are expected to report all services using the most up-to-date, industry-standard
procedures and diagnosis codes at the time of the service.
ICD-10
Diagnosis
Codes
Description: Diagnoses Requiring Prior Authorization for Any Treatment
Plan note: The initial medical evaluation does NOT require prior authorization when it is a
component of a new patient office visit and conducted by a participating oral and
maxillofacial surgeon or participating otolaryngologist and bills with one of the following
diagnosis codes.
M26.601
Right temporomandibular joint disorder
M26.602
Left temporomandibular joint disorder
M26.603
Bilateral temporomandibular joint disorder
M26.609
Unspecified temporomandibular joint disorder
M26.611
Adhesions and ankylosis of right temporomandibular joint
M26.612
Adhesions and ankylosis of left temporomandibular joint
M26.613
Adhesions and ankylosis of bilateral temporomandibular joint
M26.619
Adhesions and ankylosis of temporomandibular joint, unspecified side
Temporomandibular Joint Disorder Treatment
6 of 16
M26.621
Arthralgia of right temporomandibular joint
M26.622
Arthralgia of left temporomandibular joint
M26.623
Arthralgia of bilateral temporomandibular joint
M26.629
Arthralgia of temporomandibular joint
M26.631
Articular disc disorder of right temporomandibular joint
M26.632
Articular disc disorder of left temporomandibular joint
M26.633
Articular disc disorder of bilateral temporomandibular joint
M26.639
Articular disc disorder of temporomandibular joint, unspecified side
M26.641
Arthritis of right temporomandibular joint
M26.642
Arthritis of left temporomandibular joint
M26.643
Arthritis of bilateral temporomandibular joint
M26.649
Arthritis of unspecified temporomandibular joint
M26.651
Arthropathy of right temporomandibular joint
M26.652
Arthropathy of left temporomandibular joint
M26.653
Arthropathy of bilateral temporomandibular joint
M26.659
Arthropathy of unspecified temporomandibular joint
M26.69
Other specified disorders of temporomandibular joint
References
Abboud WA, Givol N, Yahalom R. Arthroscopic lysis and lavage for internal derangement of the
temporomandibular joint. Ann Maxillofac Surg. 2015 Jul-Dec;5(2):158-62. doi: 10.4103/2231-
0746.175754. PMID: 26981463.
Abboud WA, Yarom N, Yahalom R, Joachim M, Reiter S, Koren O, Elishoov H. Comparison of two
physiotherapy programs for rehabilitation after temporomandibular joint arthroscopy. Int J Oral
Maxillofac Surg. 2018 Jun;47(6):755-61. doi: 10.1016/j.ijom.2017.10.019. Epub 2017 Nov 15. PMID:
29150380.
Abboud W, Nadel S, Yarom N, Yahalom R. Arthroscopy of the Temporomandibular Joint for the
Treatment of Chronic Closed Lock. Isr Med Assoc J. 2016 Jul;18(7):397-400. PMID: 28471560.
Abboud W, Yahalom R, Leiba M, Greenberg G, Yarom N. Temporomandibular joint involvement in
patients with multiple myeloma-a retrospective study. Int J Oral Maxillofac Surg. 2016
Dec;45(12):1545-50. doi: 10.1016/j.ijom.2016.06.014. Epub 2016 Jul 1. PMID: 27377681.
Al-Baghdadi M, Durham J, Steele J. Timing interventions in relation to temporomandibular joint closed
lock duration: a systematic review of ‘locking duration.’ J Oral Rehabil. 2014 Jan;41(1):24-58. doi:
10.1111/joor.12126. Epub 2014 Jan 7. PMID: 24393132.
Al-Morass EA. Open versus arthroscopic surgery for the management of internal derangement of the
temporomandibular joint: a meta-analysis of the literature. Int J Oral Maxillofac Surg. 2015
Jun;44(6):763-70. doi: 10.1016/j.ijom.2015.01.024. Epub 2015 Feb 18. PMID: 25701306.
Temporomandibular Joint Disorder Treatment
7 of 16
The American Academy of Orofacial Pain (AAOP). Orofacial Pain: Guidelines for Assessment,
Diagnosis and Management. Fifth Edition. 2013.
American Association of Oral and Maxillofacial Surgeons (AAOMS). Parameters of Care Version 6:
Clinical Practice Guidelines for Oral and Maxillofacial Surgery. 2017.
American Dental Association. Clinical Practice Guidelines.
American Society of Temporomandibular Joint Surgeons (ASTMJS). Guidelines.
American Society of Temporomandibular Joint Surgeons (ASTMJS). Guidelines for diagnosis and
management of disorders involving the temporomandibular joint and related musculoskeletal
structures. Cranio. 2003 Jan;21(1):68-76. PMID: 12555934.
Blasco-Bonora PM, Martín-Pintado-Zugasti A. Effects of myofascial trigger point dry needling in
patients with sleep bruxism and temporomandibular disorders: a prospective case series. Acupunct
Med. 2017 Mar;35(1):69-74. doi: 10.1136/acupmed-2016-011102. Epub 2016 Oct 3. PMID: 27697769.
Butts R, Dunning J, Pavkovich R, Mettille J, Mourad F. Conservative management of
temporomandibular dysfunction: A literature review with implications for clinical practice guidelines
(Narrative review part 2). J Bodyw Mov Ther. 2017 Jul; 21(3):541-548. doi: 10.1016/j.jbmt.2017.05.021.
Epub 2017 Jun 1. PMID: 28750962.
Centers for Medicare & Medicaid Services (CMS). Manuals. Publication # 100-02. Medicare Benefit
Policy Manual.
Centers for Medicare & Medicaid Services (CMS). Manuals. Publication # 100-03. Medicare National
Coverage Determinations (NCD) Manual.
Centers for Medicare & Medicaid Services (CMS). Medicare Coverage Database (MCD).
Centers for Medicare & Medicaid Service (CMS). National Coverage Determination (NCD) for
Assessing Patient's Suitability for Electrical Nerve Stimulation Therapy 160.7.1. Version 2. 2006 Jun 19.
Centers for Medicare & Medicaid Service (CMS). National Coverage Determination (NCD) for
Manipulation 150.1. Effective date not posted.
Centers for Medicare & Medicaid Service (CMS). National Coverage Determination (NCD) for
Transcutaneous Electrical Nerve Stimulators (TENS) 280.13. Version 2. 2012 Jun 8.
Centers for Medicare & Medicaid Services (CMS). Transmittals.
Chebbi R, Khalifa HB, Dhidah M. Temporomandibular joint disorder in systemic sclerosis: a case report.
Pan Afr Med J. 2016 Nov 16;25:164. doi: 10.11604/pamj.2016.25.164.10432. eCollection 2016.
Temporomandibular Joint Disorder Treatment
8 of 16
PMID: 28292126.
Chen YW, Chiu YW, Chen CY, Chuang SK. Botulinum toxin therapy for temporomandibular joint
disorders: a systematic review of randomized controlled trials. Int J Oral Maxillofac Surg. 2015
Aug;44(8):1018-26. doi: 10.1016/j.ijom.2015.04.003. Epub 2015 Apr 25. PMID: 25920597.
Cömert Kiliç S, Güngörmüs M. Is dextrose prolotherapy superior to placebo for the treatment of
temporomandibular joint hypermobility? A randomized clinical trial. Int J Oral Maxillofac Surg. 2016
Jul;45(7):813-9. doi: 10.1016/j.ijom.2016.01.006. Epub 2016 Feb 2. PMID: 2684679.
Commonwealth of Massachusetts. Division of Insurance (DOI) Bulletins.
Commonwealth of Massachusetts. MassHealth Provider Bulletins.
Commonwealth of Massachusetts. MassHealth Provider Manuals.
Commonwealth of Massachusetts. MassHealth Transmittal Letters.
de Freitas RF, Ferreira MÂ, Barbosa GA, Calderon PS. Counselling and self-management therapies for
temporomandibular disorders: a systematic review. J Oral Rehabil. 2013 Nov;40(11):864-74. doi:
10.1111/joor.12098. Epub 2013 Sep 18. PMID: 24102692.
de Leeuw R, Klasser GD. Orofacial Pain: Guidelines for Assessment, Diagnosis, and Management, Fifth
Edition. 2013.
Gauer RL, Semidey MJ. Diagnosis and Treatment of Temporomandibular Disorders. Am Fam
Physician. 2015 Mar 15; 91(6):378-86. PMID: 25822556.
Gurung T, Singh RK, Mohammad S, Pal US, Mahdi AA, Kumar M. Efficacy of arthrocentesis versus
arthrocentesis with sodium hyaluronic acid in temporomandibular joint osteoarthritis: A comparison.
Natl J Maxillofac Surg. 2017 Jan-Jun;8(1):41-9. doi: 10.4103/njms.NJMS_84_16. PMID: 28761275.
Hayes. Comparative Effectiveness Review. Comparative Effectiveness Review of Dry Needling for
Indications Other than Neck or Trapezius Muscle Pain in Adults. Dallas, TX: Hayes; 2017 Jun 22. Annual
Review 2021 Jun 30.
Huang IY, Chen CM, Kao YH, Chen CM, Wu CW. Management of long-standing mandibular dislocation.
Int J Oral Maxillofac Surg. 2011 Aug;40(8):810-4. doi: 10.1016/j.ijom.2011.02.031. Epub 2011 Apr 6. PMID:
21474286.
Huang IY. A simple method to expand the joint space for TMJ surgery. Int J Oral Maxillofac Surg. 2011
Sep;40(9):983-4. doi: 10.1016/j.ijom.2011.04.011. Epub 2011 May 23. PMID: 21602029.

Temporomandibular Joint Disorder Treatment
9 of 16
Ivorra-Carbonell L, Montiel-Company JM, Almerich-Silla JM, Paredes-Gallardo V, Bellot-Arcis C.
Impact of functional mandibular advancement appliances on the temporomandibular joint - a
systematic review. Med Oral Patol Oral Cir Buccal. 2016 Sep; 21(5):e565-72. doi: 10.4317/
medoral.21180. PMID: 27475694.
Korkmaz YT, Altıntas NY, Korkmaz FM, Candırlı C, Coskun U, Durmuslar MC. Is Hyaluronic Acid Injection
Effective for the Treatment of Temporomandibular Joint Disc Displacement With Reduction? J Oral
Maxillofac Surg. 2016 Sep;74(9):1728-40. doi: 10.1016/j.joms.2016.03.005. Epub 2016 Mar 15. PMID:
27058964.
Liu F, Steinkeler A. Epidemiology, diagnosis, and treatment of temporomandibular disorders. Dent Clin
North Am. 2013 Jul;57(3):465-79. doi: 10.1016/j.cden.2013.04.006. PMID: 23809304.
MacIntosh RB, Shivapuja PK, Naqvi R. Scleroderma and the temporomandibular joint: reconstruction in
2 variants. J Oral Maxillofac Surg. 2015 Jun;73(6):1199-210. doi: 10.1016/j.joms.2014.12.012. Epub 2014
Dec 17. PMID: 25795177.
Majumdar SK, Krishna S, Chatterjee A, Chakraborty R, Ansari N. Single Injection Technique
Prolotherapy for Hypermobility Disorders of TMJ Using 25% Dextrose: A Clinical Study. J Maxillofac
Oral Surg. 2017 Jun;16(2):226-30. doi: 10.1007/s12663-016-0944-0. Epub 2016 Jul 25. PMID:
28439165.
Manfredini D. Current Concepts on Temporomandibular Disorders. Quintessence Publishers 2010.
Manfredini D, Favero L, Michieli M, Salmaso L, Cocilovo F, Guarda-Nardini L. An assessment of the
usefulness of jaw kinesiography in monitoring temporomandibular disorders: correlation of treatment-
related kinesiographic and pain changes in patients receiving temporomandibular joint injections. J Am
Dent Assoc. 2013 Apr;144(4):397-405. PMID: 23543694.
Martins WD, Ribas Mde O, Bisinelli J, França BH, Martins G. Recurrent dislocation of the
temporomandibular joint: a literature review and two case reports treated with eminectomy. Cranio.
2014 Apr; 32(2):110-7. doi: 10.1179/0886963413Z.00000000017. PMID: 24839722.
Mina R, Melson P, Powell S, Rao M, Hinze C, Passo M, Graham TB, Brunner HI. Effectiveness of
dexamethasone iontophoresis for temporomandibular joint involvement in juvenile idiopathic arthritis.
Arthritis Care Res (Hoboken). 2011 Nov;63(11):1511-6. doi: 10.1002/acr.20600. PMID: 22034112.
Monje-Gil F, Nitzan D, González-Garcia R. Temporomandibular joint arthrocentesis. Review of the
literature. Med Oral Patol Oral Cir Buccal. 2012 July;17(4): e575–81. PMID: 22322493.
New Hampshire Department of Health and Human Services. Billing Manuals.
New Hampshire Department of Health and Human Services. Provider Notices.

Temporomandibular Joint Disorder Treatment
10 of 16
Niibo P, Pruunsild C, Voog-Oras Ü, Nikopensius T, Jagomägi T, Saag M. Contemporary management of
TMJ involvement in JIA patients and its orofacial consequences. EPMA J. 2016 Jun 2;7:12. doi:
10.1186/s13167-016-0061-7. eCollection 2016. PMID: 27257443.
O’Connor RC, Fawthrop F, Salha R, Sidebottom AJ. Management of the temporomandibular joint in
inflammatory arthritis: Involvement of surgical procedures. Eur J Rheumatol. 2017 Jun;4(2):151–6.
doi: 10.5152/eurjrheum.2016.035. Epub 2017 Feb 23. PMID: 28638693.
Politi M, Sembronio S, Robiony M, Costa F, Toro C, Undt G. High condylectomy and disc repositioning
compared to arthroscopic lysis, lavage, and capsular stretch for the treatment of chronic closed lock of
the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007 Jan;103(1):27-
33. Epub 2006 Jul 27. PMID: 17178490.
Prechel U, Ottl P, Ahlers OM, Neff A. The Treatment of Temporomandibular Joint Dislocation. Dtsch
Arztebl Int. 2018 Feb 2; 115(5):59-64. doi: 10.3238/arztebl.2018.0059. PMID: 29439762.
Rigon M, Pereira LM, Bortoluzzi MC, Loguercio AD, Ramos AL, Cardoso JR. Arthroscopy for
Temporomandibular Disorders. Cochrane Database Syst Rev. 2011 May 11 ;(5):CD006385. doi:
10.1002/14651858.CD006385.pub2. PMID: 21563153.
Rodrigues-Bigaton D, Dibai Filho AV, Costa AC, Packer AC, de Castro EM. Accuracy and reliability of
infrared thermography in the diagnosis of arthralgia in women with temporomandibular disorder. J
Manipulative Physiol Ther. 2013 May;36(4):253-8. doi: 10.1016/j.jmpt.2013.04.006. Epub 2013 May 27.
PMID: 23719519.
Rodrigues PC, da Mota AS, Pereira JR, Stuginski-Barbosa J. Management of painful
temporomandibular joint clicking with different intraoral devices and counseling: a controlled study. J
Appl Oral Sci. 2015 Sep-Oct;23(5):529–35. doi: 10.1590/1678-775720140438. PMCID: PMC4621948.
Schiffman EL, Velly AM, Look JO, Hodges JS, Swift JQ, Decker KL, Anderson QN, Templeton RB,
Lenton PA, Kang W, Fricton JR. Effects of four treatment strategies for temporomandibular joint
closed lock. Int J Oral Maxillofac Surg. 2014 Feb;43(2):217-26. doi: 10.1016/j.ijom.2013.07.744. Epub
2013 Sep 14. PMID: 24042068.
Schiffman E, Ohrbach R. Executive summary of the Diagnostic Criteria for Temporomandibular
Disorders for clinical and research applications. J Am Dent Assoc. 2016 Jun;147(6):438-45.
doi: 10.1016/j.adaj.2016.01.007. PMID: 26922248.
Scrivani SJ, Khawaja SN, Bavia PF. Nonsurgical Management of Pediatric Temporomandibular Joint
Dysfunction. Oral Maxillofac Surg Clin North Am. 2018 Feb;30(1):35-45. doi: 10.1016/
j.coms.2017.08.001. PMID: 29153236.
Shukla D, Muthusekhar MR. Efficacy of low-level laser therapy in temporomandibular disorders: A
systematic review. Natl J Maxillofac Surg. 2016 Jan-Jun;7(1):62–6. doi: 10.4103/0975-5950.196127.
Temporomandibular Joint Disorder Treatment
11 of 16
PMID: 28163481.
U. S. Food & Drug Administration (FDA). Medical Devices. 510(k) Clearances.
U.S. Food & Drug Administration (FDA). 510(k) Summary for the Biowave Deepwave Percutaneous
Neuromodulation Pain Therapy System. 2006 Jul 19.
U.S. Food & Drug Administration (FDA). 510(k) Summary of Safety and Effectiveness. Vertis
Neuroscience, Inc. Percutaneous Neuromodulation Therapy (PNT) ™ Control Unit and Accessories.
2002.
U. S. Food & Drug Administration (FDA). Medical Devices. Device Registration and Listing.
Wieckiewicz M, Boening K, Wiland P, Shiau YY, Paradowska-Stolarz A. Reported concepts for the
treatment modalities and pain management of temporomandibular disorders. J Headache Pain.
2015;16:106. doi: 10.1186/s10194-015-0586-5. Epub 2015 Dec 7. PMID: 26644030.
Xu GZ, Jia J, Jin L, Li JH, Wang ZY, Cao DY. Low-Level Laser Therapy for Temporomandibular
Disorders: A Systematic Review with Meta-Analysis. Pain Res Manag. 2018 May 10;2018:4230583. doi:
10.1155/2018/4230583. eCollection 2018. PMID: 29861802.
Zhang C, Wu JY, Deng DL, He BY, Tao Y, Niu YM, Deng MH. Efficacy of splint therapy for the
management of temporomandibular disorders: a meta-analysis. Oncotarget. 2016 Dec
20;7(51):84043-53. doi: 10.18632/oncotarget.13059. PMID: 27823980.
Next Review Date
07/01/23
Authorizing Entity
MPCTAC
Appendix
Appendix: Policy History
Disclaimer Information:
Plan refers to Boston Medical Center Health Plan, Inc. which operates under the trade name WellSense Health Plan. Medical
Policies are the Plan’s guidelines for determining the medical necessity of certain services or supplies for purposes of
determining coverage. These Policies may also describe when a service or supply is considered experimental or
investigational, or cosmetic. In making coverage decisions, the Plan uses these guidelines and other Plan Policies, as well as
the Member’s benefit document, and when appropriate, coordinates with the Member’s health care Providers to consider the
individual Member’s health care needs.
Plan Policies are developed in accordance with applicable state and federal laws and regulations, and accrediting organization
standards (including NCQA). Medical Policies are also developed, as appropriate, with consideration of the medical necessity
Temporomandibular Joint Disorder Treatment
12 of 16
definitions in various Plan products, review of current literature, consultation with practicing Providers in the Plan’s service
area who are medical experts in the particular field, and adherence to FDA and other government agency policies. Applicable
state or federal mandates, as well as the Member’s benefit document, take precedence over these guidelines. Policies are
reviewed and updated on an annual basis, or more frequently as needed. Treating providers are solely responsible for the
medical advice and treatment of Members.
The use of this Policy is neither a guarantee of payment nor a final prediction of how a specific claim(s) will be adjudicated.
Reimbursement is based on many factors, including member eligibility and benefits on the date of service; medical necessity;
utilization management guidelines (when applicable); coordination of benefits; adherence with applicable Plan policies and
procedures; clinical coding criteria; claim editing logic; and the applicable Plan – Provider agreement.

Temporomandibular Joint Disorder Treatment
13 of 16
Appendix: Policy History
Original
Approval Date
Original Effective
Date* and Version
Policy Owner
Original Policy
Approved by
Regulatory Approval: N/A
Internal Approval:
09/09/08: Medical Policy, Criteria, and
Technology Assessment Committee
(MPCTAC)
09/30/08: Utilization Management
Committee (UMC)
10/22/08: Quality Improvement
Committee (QIC)
01/01/09
Version 1
Director of Medical
Policy as Chair of
MPCTAC
MPCTAC, QIC, and
UMC
*Effective Date for QHP Commercial Product: 01/01/12
*Effective Date for New Hampshire Medicaid Product: 01/01/13
*Effective Date for Senior Care Options Product: 01/01/16
*Effective Date for New Hampshire Medicare Advantage HMO Product: 01/01/22
Policy Revisions History
Review
Date
Summary of Revisions
Revision Effective
Date and Version
Number
Approved by
09/22/09
No criteria changes. Updated references.
Version 2
09/22/09: MPCTAC
10/28/09: QIC
09/01/10
No changes to criteria. Updated references and
coding.
Version 3
09/15/10: MPCTAC
11/22/10: QIC
09/01/11
Updated limitations and references.
Version 4
09/21/11: MPCTAC
10/26/11: QIC
07/01/12
References updated, revised language in the
Applicable Coding section, and deleted four-
digit diagnosis code 524.6.
Version 5
07/18/12: MPCTAC
08/22/12: QIC
07/01/13
Review for effective date 11/01/13. Updated
references. Added criteria for medical
evaluation of TMJ disorders. Reformatted,
revised, and added examples in the Medical
Policy Statement section. Added definition for
temporomandibular joint syndrome. Deleted
duplicate text in Clinical Background
Information section.
11/01/13
Version 6
07/17/13: MPCTAC
08/15/13: QIC
07/29/12
Off cycle review for WellSense New Hampshire
Medicaid product, revised Description of Item or
Service section, reformatted the Medical Policy
Version 7
08/03/12: MPCTAC
09/05/12: QIC
Temporomandibular Joint Disorder Treatment
14 of 16
Statement section, and updated the References
section.
01/30/14
Off cycle review for effective date 04/01/14.
Added ICD10 diagnosis code equivalents of
existing ICD9 diagnosis codes.
Version 8
01/27/14: MPCTAC
01/30/14: QIC
09/01/14
Review for effective date 01/01/15. Revised
language in the Limitations section related to
benefit coverage. Revised medical criteria in the
Medical Policy Statement and Limitations
sections. Updated references.
01/01/15
Version 9
09/17/14: MPCTAC
10/08/14: QIC
09/01/15
Annual review for effective date 01/01/16.
Revised the list of applicable products, including
removing Commonwealth Care, Commonwealth
Choice, and Employer Choice from the list of
applicable products because the products are
no longer available. Revised criteria in the
Medical Policy Statement and Limitations
sections. Updated Clinical Background
Information and References sections.
01/01/16
Version 10
09/16/15: MPCTAC
10/14/15: QIC
11/25/15
Review for effective date 01/14/16. Revised
language in the Applicable Coding section.
01/14/16
Version 11
11/25/15: MPCTAC
(electronic vote)
12/09/15: QIC
09/01/16
and
09/28/16
Review for effective date 01/01/17. Removed
ICD9 diagnosis codes. Updated Summary,
Description of Item or Service, Definitions,
Clinical Background Information, References,
and Reference to Applicable Laws and
Regulations sections. Revised criteria in the
Medical Policy Statement and Limitations
sections. Administrative changes made to
clarify language related to gender.
01/01/17
Version 12
09/21/16: MPCTAC
09/30/16: MPCTAC
(electronic vote)
10/12/16: QIC
12/05/16
Industry-wide changes to applicable ICD-10
diagnosis codes for temporo-mandibular joint
disorder effective 01/01/17.
01/01/17
Version 13
Not applicable
because industry-wide
revisions to ICD-10
diagnosis codes.
09/01/17
Review for effective date 12/01/17. Revised
criteria in the Medical Policy Statement and
Limitations sections. Updated the Policy
Summary, Definitions, References, Other
Applicable Policies, and Reference to Applicable
Laws and Regulations sections.
12/01/17
Version 14
09/20/17: MPCTAC
09/01/18
Review for effective date 12/01/18. Updated the
Clinical Background Information, References,
and Other Applicable Policies sections. Criteria
revised in the Medical Policy Statement and
Limitations sections.
12/01/18
Version 15
09/19/18: MPCTAC
12/01/18
Review for effective date 01/01/19.
Administrative change made to the Limitations
01/01/19
Version 16
12/19/18: MPCTAC
Temporomandibular Joint Disorder Treatment
15 of 16
section (removing the reference to the NH
Health Protection Program).
09/01/19
Review for effective date 12/01/19.
Administrative changes made to the Policy
Summary, Definitions, References, and
Reference to Applicable Laws and Regulations
sections. Revised criteria in the Limitations
section.
12/01/19
Version 17
09/18/19: MPCTAC
07/01/20
Review for effective date 10/01/20 to be
consistent with implementation date of
industry-wide diagnosis code updates made to
the Applicable Coding section. Administrative
changes made to the Medical Policy Statement,
References, and Other Applicable Policies
sections.
10/01/20
Version 18
07/15/20: MPCTAC
08/01/21
Review for effective date 09/01/21.
Administrative changes made to the Policy
Summary, Medical Policy Statement,
Limitations, and References sections.
09/01/21
Version 19
08/27/21: MPCTAC
(electronic vote)
11/01/21
Review for effective date 12/01/21. Adopted
new medical policy template; removed
administrative sections, the Medical Policy
Statement section renamed the Clinical Criteria
section, and the Limitations section renamed
the Limitations and Exclusions section. Added
WellSense Medicare Advantage HMO as an
applicable product effective 01/01/22.
Administrative changes made to the Policy
Summary, Clinical Criteria, Limitations and
Exclusions, Applicable Coding, and References
sections.
12/01/21
Version 20
11/17/21: MPCTAC
07/01/22
Review for effective date 08/01/22.
Administrative changes made to the Policy
Summary, Clinical Criteria, Limitations and
Exclusions, Applicable Coding, and References
sections.
08/01/22
Version 21
07/25/22: MPCTAC
(electronic vote)
08/01/22
Review for effective date 11/01/22.
Administrative changes made to the Policy
Summary section.
11/01/22
Version 22
Version 22 not
implemented and
replaced with
Version 23 as of
11/01/22
08/26/22: MPCTAC
(electronic vote)
09/01/22
Review for effective date 11/01/22. Revised the
effective date of AIM’s management of
outpatient rehabilitation services from 11/01/22
to 12/01/22 in the Policy Summary section.
11/01/22
Version 23
09/23/22: MPCTAC
(electronic vote)
Temporomandibular Joint Disorder Treatment
16 of 16
Administrative changes made to the Clinical
Criteria section.
